Experience on placenta accreta spectrum disorders and multidisciplinary way of approach in its management: a retrospective study over 2 years in a tertiary care centre
Abstract
Introduction: Placenta accreta spectrum (PAS) refers to the pathologic adherence of the placentaat the defective endometrial myometrial interface leading to defective decidualization causing life-threatening haemorrhage when attempted to separate at the time of delivery thus requiringattention for a multidisciplinary approach in its management.
Aims and objectives: To study therisk factors, antenatal diagnosis, and different management approaches, associated with placentaaccreta and also to compare the maternal and fetal outcomes by different management strategies.
Methods: A retrospective analysis was done for two years from October 2019 to October 2021 withclinically diagnosed cases of PAS. We examined antenatal risk factors favouring diagnosis,peripartum morbidity and different management approaches such as vaginal delivery and curettage,by planned or emergency hysterectomy.
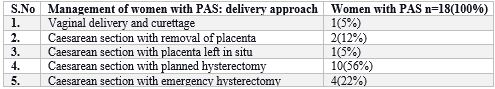
Results: 18 cases were studied showing a proportion of1.48 per 1000 live births. The median age for diagnosis was made around 33 weeks of gestationusing ultrasonography evidence in 77% of cases. Placenta accreta was seen in 66%, placenta incretain 27% and percreta in 5%. the median amount of blood loss was around 2500 ml, 83% of casesrequired blood transfusions, 44% required ICU admission and 27% of newborns required NICUadmission
Conclusion: PAS should be managed with a well-coordinated team in good settings toreduce maternal morbidity and mortality preferably at the tertiary care level
Downloads
References
2. Bhide A, Sebire N, Abuhamad A, Acharya G, Silver R (2017) Morbidly adherent placenta: the need for standardization. Ultrasound Obstet Gynecol 49(5):559–563. https://doi.org/10.1002/uog.17417
3. Garofalo A, Pilloni E, Alemanno MG et al (2019) Ultrasound accuracy in prenatal diagnosis of abnormal placentation of posterior placenta previa. Eur J Obstet Gynecol Reprod Biol 242:86– 91. https://doi.org/10.1016/j.ejogrb.2019.09.021
4. Jauniaux E, De-Campos DA. FIGO consensus guidelines on placenta accreta spectrum disorders: Introduction. Int J Gynaecol Obstet. 2018;140(3):261–4.
5. Comstock CH (2011) The antenatal diagnosis of placental attachment disorders. Curr Opin Obstet Gynecol 23(2):117–122. https ://doi.org/10.1097/GCO.0b013e328342b730
6. Mulla BM, Weatherford R, Redhunt AM et al (2019) Hemorrhagic morbidity in placenta accreta spectrum with and without placenta previa. Arch Gynecol Obstet 300(6):1601–1606. https:// doi.org/10.1007/s00404-019-05338-y
7. Couret M, Huang Y, Khoury-Collado F et al (2019) Patterns of care for women with placenta accreta spectrum. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1684471
8. Stanleigh J, Michaeli J, Armon S et al (2019) Maternal and neonatal outcomes following a proactive peripartum multidisciplinary management protocol for placenta creta spectrum as compared to the urgent delivery. Eur J Obstet Gynecol Reprod Biol 237:139– 144. https://doi.org/10.1016/j.ejogrb.2019.04.032
9. Fratto VM, Conturie CL, Ballas J et al (2019) Assessing the multidisciplinary team approaches to placenta accreta spectrum across five institutions within the University of California fetal Consortium (UCfC). J Matern Fetal Neonatal Med. https://doi. org/10.1080/14767058.2019.1676411
10. Silver RM, Fox KA, Barton JR et al (2015) Center of excellence for placenta accreta. Am J Obstet Gynecol 212(5):561–568. https ://doi.org/10.1016/j.ajog.2014.11.018
11. Cırpan T, Akdemir A, Okmen F, Hortu I, Ekici H, Imamoglu M (2019) Effectiveness of segmental resection technique in the treat- ment of placenta accreta spectrum. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1702019
12. Piñas Carrillo A, Chandraharan E (2019) Placenta accreta spec- trum: Risk factors, diagnosis and management with special reference to the Triple P procedure. Womens Health (Lond) 15:1745506519878081. https://doi.org/10.1177/1745506519 878081
13. Shih J-C, Liu K-L, Kang J, Yang J-H, Lin M-W, Yu C-U (2019) “Nausicaa” compression suture: a simple and effective alternative to hysterectomy in placenta accreta spectrum and other causes of severe postpartum haemorrhage. BJOG 126(3):412–417. https:// doi.org/10.1111/1471-0528.15410
14. Slaoui A, Talib S, Nah A et al (2019) Placenta accreta in the department of gynaecology and obstetrics in Rabat, Morocco: case series and review of the literature. Pan Afr Med J 33:86. https://doi.org/10.11604/pamj.2019.33.86.17700
15. The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine (2018) Obstetric Care Consensus No. 7: placenta accreta spectrum. Obstet Gynecol 132(6):e259–e275. https://doi.org/10.1097/AOG.0000000000 002983
16. Sentilhes L, Kayem G, Chandraharan E, Palacios-Jaraquemada J, Jauniaux E, FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: conservative management. Int J Gynaecol Obstet 140(3):291–298. https://doi.org/10.1002/ ijgo.12410
17. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, Moawad AH, Caritis SN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, Carpenter M, Peaceman AM, O'Sullivan MJ, Sibai B, Langer O, Thorp JM, Ramin SM, Mercer BM; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006 Jun;107(6):1226-32. doi: 10.1097/01.AOG.0000219750.79480.84. PMID: 16738145.
18. Jauniaux E, Bunce C, Grønbeck L, Langhoff-Roos J (2019) Preva- lence and main outcomes of placenta accreta spectrum: a system- atic review and meta-analysis. Am J Obstet Gynecol 221(3):208– 218. https://doi.org/10.1016/j.ajog.2019.01.233
19. Wu S, Kocherginsky M, Hibbard JU (2005) Abnormal placenta- tion: twenty-year analysis. Am J Obstet Gynecol 192(5):1458– 1461. https://doi.org/10.1016/j.ajog.2004.12.074
20. Allen L, Jauniaux E, Hobson S, Papillon-Smith J, Belfort MA, FIGO Placenta Accreta Diagnosis and Management Expert Con- sensus Panel (2018) FIGO consensus guidelines on placenta accreta spectrum disorders: nonconservative surgical man- agement. Int J Gynaecol Obstet 140(3):281–290. https://doi. org/10.1002/ijgo.12409
21. Jauniaux E, Chantraine F, Silver RM, Langhoff-Roos J, FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel (2018) FIGO consensus guidelines on placenta accreta spec- trum disorders: epidemiology. Int J Gynaecol Obstet 140(3):265– 273. https://doi.org/10.1002/ijgo.12407
22. Cal M, Ayres-de-Campos D, Jauniaux E (2018) International sur- vey of practices used in the diagnosis and management of placenta accreta spectrum disorders. Int J Gynaecol Obstet 140(3):307– 311. https://doi.org/10.1002/ijgo.12391
Copyright (c) 2022 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

