A study of efficacy of oral probiotics in management of cases with symptomatic white discharge per vagina in a tertiary care hospital
Abstract
Background: Urogenital infections are the most common gynecological condition constituting about 25% of outpatients. Because of higher recurrence rates and resistance to standard antimicrobials now a days the use of probiotics in augmenting normal bacterial populations is gradually achieving scientific acceptance.
Objective: Determine the efficacy of probiotics in treating women with symptomatic white discharge per vagina (WDPV), role of oral probiotics in restoring the vaginal flora.
Methods: 70 women aged between 18 to 45 yrs (mean age 35yrs) with symptomatic WDPV who are attending gynecology outpatient procedures, these patients underwent Grams stain, received antibiotics along with probiotics (L. rhamnosus GR-1 and L. fermentum RC-14) for a period of 1 week, again reviewed with repeat Grams stain.
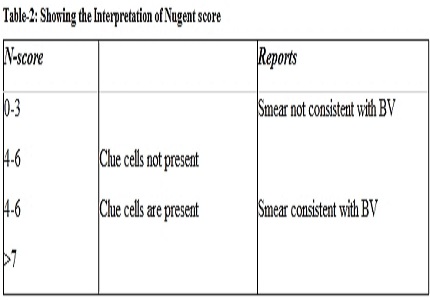
Results: Among post-treatment group 46 % of patients showed >30 organisms/100× objective. Fifty percent of patients showed counts between 5 and 30 among post-treatment, but the response in terms of symptomatic relief was about 74%. The improvement in the lactobacilli count was interpreted using Nugents scoring.
Conclusion: The combination of probiotic (L. rhamnosus GR-1 and L. fermentum RC-14) is not only safe for daily use in healthy women, but it can reduce colonization of the vagina by potential pathogenic bacteria and yeast.
Downloads
References
2. Schwebke JR, Richey CM, Weiss2 HL. Correlation of behaviors with microbiological changes in vaginal flora. J Infect Dis. 1999 Nov;180(5):1632-6. [PubMed]
3. Bruce AW, Chadwick P, Seddon JM, Vancott GF. The significance of perineal pathogens in women. J Urol. 1974 Dec;112(6):808-10.
4. Sewankambo N, Gray RH, Wawer MJ, Paxton L, McNaim D, Wabwire-Mangen F, Serwadda D, Li C, Kiwanuka N, Hillier SL, Rabe L, Gaydos CA, Quinn TC, Konde-Lule J. HIV-1 infection associated with abnormal vaginal flora morphology and bacterial vaginosis. Lancet. 1997 Aug 23;350(9077):546-50. [PubMed]
5. Reid G, Bruce AW, Beheshti M. Effect of antibiotic treatment on receptivity of uroepithelial cells to uropathogens. Can J Microbiol. 1988 Mar;34(3):327-31. [PubMed]
6. Petrof EO, Schwartz DN, Quinn JP. Urinary tract infections and a multidrug-resistant Escherichia coli clonal group. N Engl J Med. 2002 Feb 14;346(7):535-6. [PubMed]
7. Ellis AK, Verma S. Quality of life in women with urinary tract infections: is benign disease a misnomer? J Am Board Fam Pract. 2000 Nov-Dec;13(6):392-7. [PubMed]
8. FAO/WHO. Evaluation of health and nutritional properties of powder milk and live lactic acid bacteria. Food and Agriculture Organization of the United Nations and World Health Organization Report 2001.
9. FAO/WHO. Guidelines for the evaluation of probiotics in food. Report of a joint FAO/WHO Working Group 2002.
10. Reid G, Bruce AW, Fraser N, Heinemann C, Owen J, Henning B. Oral probiotics can resolve urogenital infections. FEMS Immunol Med Microbiol. 2001 Feb;30(1):49-52.
11. Reid G, Beuerman D, Heinemann C, Bruce AW. Probiotic Lactobacillus dose required to restore and maintain a normal vaginal flora. FEMS Immunol Med Microbiol. 2001 Dec;32(1):37-41. [PubMed]
12. Bijeta, Shreshtha Singh. Incidence of bacterial vaginosis in patients with idiopathic preterm labour. Int J Reprod Contracept Obstet Gynecol. 2015; 4(3): 641-646.
13. Champagne CP, Ross RP, Saarela M, Hansen KF, Charalampopoulos D. Recommendations for the viability assessment of probiotics as concentrated cultures and in food matrices. Int J Food Microbiol. 2011 Oct 3;149(3):185-93. doi: 10.1016/j.ijfoodmicro.2011.07.005. Epub 2011 Jul 14. [PubMed]
14. Wagner RD, Johnson SJ. Probiotic lactobacillus and estrogen effects on vaginal epithelial gene expression responses to Candida albicans. J Biomed Sci. 2012 Jun 20;19:58. doi: 10.1186/1423-0127-19-58. [PubMed]
15. Larsson et al. Extended antimicrobial treatment of bacterial vaginosis combined with human lactobacilli to find the best treatment and minimize the risk of relapse.BMJ Infectious Diseases.2011;11:223.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

