Pregnancy outcome among gestational diabetes mellitus patients
Abstract
Background and Aim: Though not all babies have birth defects there is still a high probability of congenital defects if the glucose level is not under control during pregnancy and also increased morbidity in terms of hypoglycemia, hyperbilirubinemia, and respiratory distress syndrome warranting NICU admissions. The objective of this study was to find out the maternal and perinatal outcome in patients with gestational diabetes mellitus.
Material and Methods: An observational study was conducted among 400 pregnant women who came for antenatal checkups attending the OPD of the department of obstetrics and gynecology, the tertiary care institute of Gujarat, from June 2012 to November 2013. A detailed history including maternal age, parity, BMI, and clinical examination along with antenatal checkup was done.
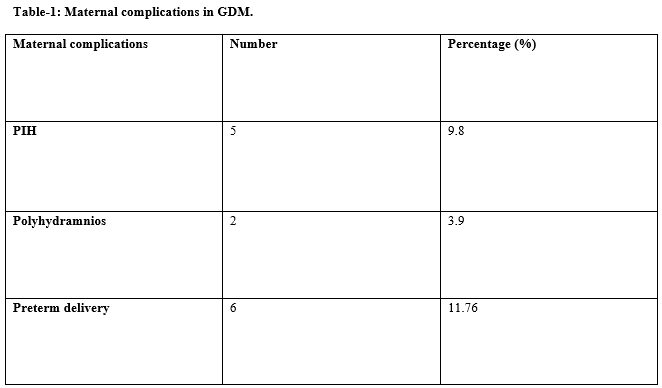
Results: Out of 400 antenatal women tested for OGTT using 75 grams of glucose, about 12.75% (51) of antenatal women developed GDM. Out of 51 GDM mothers, about 10% ie.,5 antenatal women had pregnancy-induced hypertension and only 2 developed polyhydramnios and preterm delivery in 11.76% of antenatal women with GDM Out of 51 babies, 19.6% of them had respiratory distress syndrome, 7.8% of the babies requiring NICU admissions because of hypoglycemia, hyperbilirubinemia, and hypocalcemia.
Conclusion: Gestational diabetes mellitus was once thought to be a mild condition but now it carries significant short-term and long-term implications for the women and their offspring. Screening for diabetes is mandatory in preventing complications as strict glycemic control is necessary for preventing macrosomia and unexplained stillbirths.
Downloads
References
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(suppl 1):s81-S90. doi: 10.2337/dc14-S081.
Hunt KJ, Schuller KL. The increasing prevalence of diabetes in pregnancy. Obstet Gynecol Clin N Am. 2007;34(2):173-199. doi: 10.1016/j.ogc.2007.03.002.
Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(suppl 2):s141–S146. doi: 10.2337/dc07-s206.
Moses RG, Morris GJ, Petocz P, San Gil F, Garg D. The impact of potential new diagnostic criteria on the prevalence of gestational diabetes mellitus in Australia. Med J Aust. 2011;194(7):338-340. doi: 10.5694/j.1326-5377.2011.tb03001.x.
Yang X, Hsu-Hage B, Zhang H, Zhang C, Zhang Y, Zhang C. Women with impaired glucose tolerance during pregnancy have significantly poor pregnancy outcomes. Diabetes Care. 2002;25(9):1619-1624. doi: 10.2337/diacare.25.9.1619.
Langer O, Yogev Y, Most O, Xenakis EMJ. Gestational diabetes: the consequences of not treating. Obstet Gynecol. 2005;192(4):989-997. doi: 10.1016/j.ajog.2004.11.039.
Sermer M, Naylor CD, Gare DJ, Kenshole AB, Ritchie J, Farine D, et al. Impact of increasing carbohydrate intolerance on maternal-fetal outcomes in 3637 women without gestational diabetes: the Toronto tri-hospital gestational diabetes project. Obstet Gynecol. 1995;173(1):146-156. doi: 10.1016/0002-9378(95)90183-3.
Brown J, Alwan NA, West J, Brown S, Mckinlay CJ, Farrar D, Crowther CA. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database Syst Rev. 2017;5:cd01197. doi: 10.1002/14651858.CD011970.
Casey BM, Lucas MJ, McIntire DD, Leveno KJ. Pregnancy outcomes in women with gestational diabetes compared with the general obstetric population. Obstet Gynecol. 1997;90(6):869-873. doi: 10.1016/s0029-7844(97)00542-5.
Joffe GM, Esterlitz JR, Levine RJ, Clemens JD, Ewell MG, Sibai BM, et al. The relationship between abnormal glucose tolerance and hypertensive disorders of pregnancy in healthy nulliparous women. Am J Obstet Gynecol. 1998;179(4):1032-1037. doi: 10.1016/s0002-9378(98)70210-8.
Yogev Y, Xenakis EM, Langer O. The association between preeclampsia and the severity of gestational diabetes: the impact of glycemic control. Am J Obstet Gynecol. 2004;191(5):1655-1660. doi: 10.1016/j.ajog.2004.03.074.
Suhonen L, Teramo K. Hypertension and pre-eclampsia in women with gestational glucose intolerance. Acta Obstet Gynecol Scand. 1993;72(4):269-272. doi: 10.3109/00016349309068036.
Jensen DM, Sørensen B, Feilberg-Jørgensen N, Westergaard J, Beck-Nielsen H. Maternal and perinatal outcomes in 143 Danish women with gestational diabetes mellitus and 143 controls with a similar risk profile. Diabetic Med. 2000;17(4):281-286. doi: 10.1046/j.1464-5491.2000.00268.x.
Jacobson JD, Cousins L. A population-based study of maternal and perinatal outcome in patients with gestational diabetes. Am J Obstet Gynecol. 1989;161(4):981-986. doi: 10.1016/0002-9378(89)90767-9.
Naylor CD, Sermer M, Chen E, Sykora K. Cesarean delivery in relation to birth weight and gestational glucose tolerance: pathophysiology or practice style? JAMA. 1996;275(15):1165-1170.
Yogev Y, Ben-Haroush A, Chen R, Glickman H, Kaplan B, Hod M. Active induction management of labor for diabetic pregnancies at term; mode of delivery and fetal outcome—a single center experience. Eur J Obstet Gynecol Reprod Biol. 2004;114(2):166-170. doi: 10.1016/j.ejogrb.2003.10.017.
Saxena P, Tyagi S, Prakash A, Nigam A, Trivedi SS. Pregnancy outcome of women with gestational diabetes in a tertiary level hospital of north India. Soc Med. 2011;36(2):120. doi: 10.4103/0970-0218.84130.
Gascho CLL, Leandro DMK. e Silva TR, Silva JC. Predictors of cesarean delivery in pregnant women with gestational diabetes mellitus. Revista Brasileira de Ginecologia e Obstet/RBGO Gynecol Obstet. 2017;39(02):60-65. doi: 10.1055/s-0037-1598644.
Abu-Heija AT, Al-Bash M, Mathew M. Gestational and pregestational diabetes mellitus in Omani women: comparison of obstetric and perinatal outcomes. Sultan Qaboos University Med J. 2015;15(4):e496. doi: 10.18295/squmj.2015.15.04.009.
McMahon M, Ananth C, Liston R. Gestational diabetes mellitus. Risk factors, obstetric complications and infant outcomes. J Reprod Med. 1998;43(4):372-378.
Gasim T. Gestational diabetes mellitus: maternal and perinatal outcomes in 220 Saudi women. Oman Med J. 2012;27(2):140. doi: 10.5001/omj.2012.29.
Peticca P, Keely EJ, Walker MC, Yang Q, Bottomley J. Pregnancy outcomes in diabetes subtypes: how do they compare? A province-based study of Ontario, 2005–2006. J Obstet Gynaecol Canada. 2009;31(6):487-496. doi: 10.1016/s1701-2163(16)34210-4.
Tan PC, Ling LP, Omar SZ. The 50-g glucose challenge test and pregnancy outcome in a multiethnic Asian population at high risk for gestational diabetes. Int J Gynecol Obstet. 2009;105(1):50-55. doi: 10.1016/j.ijgo.2008.11.038.
Köck K, Köck F, Klein K, Bancher-Todesca D, Helmer H. Diabetes mellitus and the risk of preterm birth with regard to the risk of spontaneous preterm birth. J Maternal-Fetal Neonatal Med. 2010;23(9):1004-1008. doi: 10.3109/14767050903551392.
Bhat M, Ramesha K, Sarma SP, Menon S, Kumar SG. Outcome of gestational diabetes mellitus from a tertiary referral Center in South India: a case– control study. J Obstet Gynecol India. 2012;62(6):644-649. doi: 10.1007/s13224-012-0226-9.
Weinert LS. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: Comment to the International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Diabetes Care. 2010;33(3):e97. doi: 10.2337/dc10-0719.
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcomes. N Engl J Med. 2008;358:1991-2002. doi: 10.1056/NEJMoa0707943.
Davey RX, Hamblin PS. Selective versus universal screening for gestational diabetes mellitus: An evaluation of predictive risk factors. Med J Aust. 2001;174(3):118-121. doi: 10.5694/j.1326-5377.2001.tb143181.x.
Dashe JS, Nathan L, McIntire DD et al. Correlation between amniotic fluid glucose concentration and amniotic fluid volume in pregnancy complicated by diabetes. Am J Obstet Gynecol. 2000;182(4):901-904. doi: 10.1016/s0002-9378(00)70343-7.
DeBoer T, Wewerka S, Bauer PJ, Georgieff MK, Nelson CA. Explicit memory performance in infants of diabetic mothers at 1 year of age. Dev Med Child Neurol. 2005;47(8):525-531. doi: 10.1017/s0012162205001039.
Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004; 52:707-711.
Savitri D Kabade, Durgaprasad M Kabade, Elizabeth Wilson, Karthik SL, Lavanya K. Study of prevalence and outcome of gestational diabetes mellitus at a tertiary care hospital in North Karnataka. Int J Contemp Med Res. 2017;4(2):325-328.
Shridevi AS, Prabhudev P, Bhovi MR. A clinical study of prevalence of gestational diabetes mellitus and associated risk factors at a tertiary care centre in Karnataka, India. Int J Reprod Contracept Obstet Gynecol. 2015;4(6):1840-1845. doi: 10.18203/2320-1770.ijrcog201.
Wahi P, Dogra V, Jandial K, Bhagat R, Gupta R, Gupta S, et al. Prevalence of Gestational Diabetes Mellitus (GDM) and its Outcomes in Jammu Region. J Assoc Physicians India. 2011;59:227-230.
Reece EA, Leuizamon G, Wiznitzer A. Gestational diabetes: the need for a common ground. The Lancet. 2009;373(9677):1789-1797. doi: 10.1016/S0140-6736(09)60515-8.
Al-Hakeem MM. Pregnancy outcome of gestational diabetic mothers: experience in a tertiary care centre. J Fami Comm Med. 2006;13(2):55-59.
Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B, Aktary WM, Pasichnyk D, Seida JC, Donovan L. Screening and diagnosing gestational diabetes mellitus. Evid Rep Technol Assess (Full Rep). 2012;(210):1-327.
Gasim T. Gestational diabetes mellitus: maternal and perinatal outcomes in 220 Saudi women. Oman Med J. 2012;27(2):140-144. doi: 10.5001/omj.2012.29.
Nair VG, Sandhu GS, Biswas M, Bhalla R. Evaluation of the incidence and outcome of gestational diabetes mellitus using the current international consensus guidelines for diagnosing hyperglycemia in pregnancy. Int J Reprod Contracept Obstet Gynecol. 2016;5(10):336:1-6. doi: 10.18203/2320-1770.ijrcog20163159.
Langer O, Rodriguez DA, Xenakis EM, McFarland MB, Berkus MD, Arredondo F. Intensified versus conventional management of gestational diabetes. Am J Obstet Gynaecol. 1994;170(4):1036-1047. doi: 10.1016/S0002-9378(94)70097-4.
Jovanovic-peterson L, Peterson CM. New strategies for the treatment of gestational diabetes. Israel J Med Sci.1991;27(8-9):510-515.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

