Use of Low Dos Aspirin in Women with Increased Risk of Preeclampsia
Abstract
Introduction: The role of aspirin in the primary or secondary prevention of preeclampsia has been the subject of numerous studies and great controversy. Our aim reports on LDA usage rates by women with an increased PE risk, as well as on determinants and reasons given for use and non‐use.
Material and Method: In this multicenter, double-blind, placebo-controlled trial, the current study randomly assigned 2100 women with singleton pregnancies who were at high risk for preterm preeclampsia to receive aspirin, at a dose of 150 mg per day, or placebo from 11 to 14 weeks of gestation until 36 weeks of gestation. The primary outcome was delivery with preeclampsia before 37 weeks of gestation. The analysis was performed according to the intention-to-treat principle.
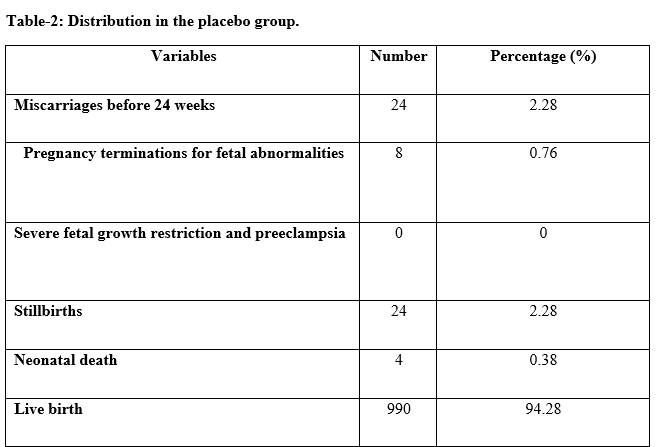
Results: Preterm preeclampsia occurred in 13 participants (1.6%) in the aspirin group, as compared with 35 (4.3%) in the placebo group (odds ratio in the aspirin group, 0.38; 95% confidence interval, 0.20 to 0.74; P=0.004). Results were materially unchanged in a sensitivity analysis that took into account participants who had withdrawn or were lost to follow-up.
Conclusion: This randomized trial showed that among women with singleton pregnancies who were identified using first-trimester screening as being at high risk for preterm preeclampsia, the administration of aspirin at a dose of 150 mg per day from 11 to 14 weeks of gestation until 36 weeks of gestation resulted in a significantly lower incidence of preterm preeclampsia than that with placebo.
Downloads
References
Navaratnam K, Alfirevic A, Alfirevic Z. Low dose aspirin and pregnancy: how important is aspirin resistance?. Int J Obstet Gynaecol. 2016;123(9):1481-1487. doi: 10.1111/1471-0528.13914.
Russo I, Penna C, Musso T, Popara J, Alloatti G, Cavalot F, et al. Diabetes and myocardial ischemia/reperfusion injury. Cardiovasc Diabetol. 2017;16:71. doi: 10.1186/s12933-017-0550-6.
Atallah A, Lecarpentier E, Goffinet F, Doret-Dion M, Gaucherand P, Tsatsaris V. Aspirin for prevention of preeclampsia. Drugs. 2017;77(17):1819-1831. doi: 10.1007/s40265-017-0823-0.
Bij de Weg JM, Abheiden CN, de Boer MA, de Groot C, de Vries JI. Patients’ perspective on aspirin during pregnancy: a survey. Hypertens Pregnancy. 2020;9(4):371-378. doi: 10.1080/10641955.2020.1777299.
Brown MA, Lindheimer MD, de Swiet M, Assche AV, Moutquin J-M: The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertens Pregnancy. 2001;20(1):IX-XIV. doi: 10.1081/PRG-100104165.
Uzan J, Carbonnel M, Piconne O, Asmar R, Ayoubi J-M. Pre-eclampsia: pathophysiology, diagnosis, and management. Vasc Health Risk Manag. 2011;7:467-474. doi: 10.2147/VHRM.S20181.
Prual A, Bouvier-Colle M-H, Bernis Ld, Breart G. Severe maternal morbidity from direct obstetric causes in West Africa: incidence and case fatality rates. Bull World Health Organ. 2000;78(5):593-602.
Loussert L, Vidal F, Parant O, Hamdi SM, Vayssiere C, Guerby P. Aspirin for prevention of preeclampsia and fetal growth restriction. Prenat Diagn. 2020;40(5):519-527. doi: 10.1002/pd.5645.
Wertaschnigg D, Reddy M, Mol BW, da Silva Costa F, Rolnik DL. Evidence-Based Prevention of Preeclampsia: Commonly Asked Questions in Clinical Practice. J Pregnancy. 2019. doi: 10.1155/2019/2675101.
Warner TD, Nylander S, Whatling C. Anti‐platelet therapy: cyclo‐oxygenase inhibition and the use of aspirin with particular regard to dual anti‐platelet therapy. Brit J Clin Pharmacol. 2011;72(4):619-633. doi: 10.1111/j.1365-2125.2011.03943.x.
Zacharias-Millward N, Menter DG, Davis JS, Lichtenberger L, Hawke D, Hawk E, et al. Beyond COX-1: the effects of aspirin on platelet biology and potential mechanisms of chemoprevention. Cancer Metastasis Rev. 2017;36(2):289-303. doi: 10.1007/s10555-017-9675-z.
Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116(2 pt 1):402-414. doi: 10.1097/AOG.0b013e3181e9322a.
Rotchell YE, Cruickshank JK, Gay MP, Griffiths J, Stewart A, Farrell B, et al. Barbados Low Dose Aspirin Study in Pregnancy (BLASP): a randomised trial for the prevention of pre-eclampsia and its complications. Br J Obstet Gynaecol. 1998;105(3):286-292. doi: 10.1111/j.1471-0528.1998.tb10088.x.
Di Sessa TG, Moretti ML, Khoury A, Pulliam DA, Arheart KL, Sibai BM. Cardiac function in fetuses and newborns exposed to low-dose aspirin during pregnancy. Am J Obstet Gynecol. 1994;171(4):892-900. doi: 10.1016/S0002-9378(94)70056-7.
Schiessl B, Schneider KT, Zimmermann A, Kainer F, Friese K, Oberhoffer R. Prenatal constriction of the fetal ductus arteriosus–related to maternal pain medication? Z Geburtshilfe Neonatol. 2005;209(02):65-68. doi: 10.1055/s-2005-864116.
Wyatt-Ashmead J. Antenatal closure of the ductus arteriosus and hydrops fetalis. Pediatr Dev Pathol Off J Soc Pediatr Pathol Paediatr Pathol Soc. 2011;14(6):469-474. doi: 10.2350/07-11-0368.1.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

