Study to assess the prevalence of antiphospholipid syndrome (APS) among women with adverse pregnancy outcome in a tertiary care centre
Abstract
Introduction: Antiphospholipid syndrome is an autoimmune condition characterized by vascular thrombosis and/or pregnancy morbidity in the presence of antiphospholipid antibodies. A failure or significant delay in recognizing APS as the underlying disease entity may leave to the loss of an opportunity to prevent serious consequences of the disease particularly venous and arterial thrombotic events.
Aim of the Study: To find out the prevalence of antiphospholipid syndromeamong women with adverse pregnancy outcome in a tertiary care centre.
Methodology: Patients registered in O &G Department SAT Hospital, Medical College, Trivandrum, Kerala with adverse pregnancy outcomes meeting the inclusion and exclusion criteria were recruited for the study. They were followed up in the postnatal ward after abortion and preterm delivery as per protocol for bad obstetrics outcome evaluation. They were offered lab test in standard labs for APL Syndrome especially LAC and anti-cardiolipin antibodies IgM & IgG. Those tested positive were retested 12 weeks later also to confirm the test.
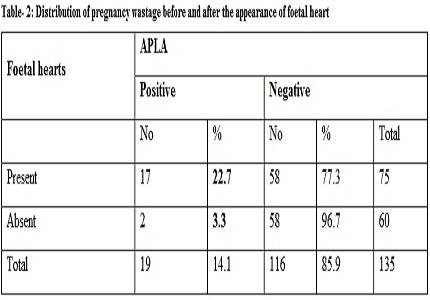
Results: In the present study, out of 216 cases of patients with adverse pregnancy outcome, 27 cases were found to be APLA positive giving a prevalence of 12.5%. In APLA positive cases LAC & ACLA were found to be positive in 11 cases each i. e 40.7% and in 5 cases both LAC & ACLA were positive i.e. 18.6%.
Conclusion: The important message is that even if a patient who is suspected clinically of APS does not fully satisfy the strict classification criteria, she may still have APS and require appropriate management including anticoagulation.
Downloads
References
2. Clowse ME, Jamison M, Myers E, James AH. A national study of the complications of lupus in pregnancy. Am J Obstet Gynecol. 2008 Aug;199(2):127.e1-6. doi: 10.1016/j.ajog.2008.03.012. Epub 2008 May 5.
3. Miyakis S1, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, Derksen RH, DE Groot PG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A,Vlachoyiannopoulos PG, Krilis SA. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006 Feb;4(2):295-306. DOI: 10.1111/j.1538-7836.2006.01753.x
4. Favaloro EJ1, Wong RC.Antiphospholipid antibodies and the antiphospholipid syndrome II: limitations, standardization, and clinical utility of laboratory testing. Semin Thromb Hemost. 2008 Jun;34(4):309-12. doi: 10.1055/s-0028-1085472. Epub 2008 Sep 23.DOI: 10.1055/s-0028-1085472
5. Yetman DL, Kutteh WH. Antiphospholipid antibody panels and recurrent pregnancy loss: prevalence of anticardiolipin antibodies compared with other antiphospholipid antibodies. Fertil Steril. 1996 Oct;66(4):540-6.
6. Oshiro BT, Silver RM, Scott JR, Yu H, Branch DW. Antiphospholipid antibodies and fetal death. Obstet Gynecol. 1996 Apr;87(4):489-93.
7. Roque H, Paidas M, Rebarber A, et al: Maternal thrombophilia is associated with second and third trimester fetal death. Am J Obstet Gynecol 184: S27, 2001.
8. Kutteh WH. Antiphospholipid antibody-associated recurrent pregnancy loss: treatment with heparin and low-dose aspirin is superior to low-dose aspirin alone. Am J Obstet Gynecol. 1996 May;174(5):1584-9.
9. Ghosh A, Ghosh M, Bhattacharya SM. Anti-phospholipid antibodies as a cause of recurrent pregnancy loss: a study in Calcutta, India. J Obstet Gynaecol. 2006 Jul;26(5):407-10.
10. Ogasawara M, Aoki K, Katano K, Aoyama T, Kajiura S, Suzumori K. Prevalence of autoantibodies in patients with recurrent miscarriages. Am J Reprod Immunol. 1999 Jan;41(1):86-90.
11 Munther A. Khamastha.E.et al. Antiphospholipid Syndrome. British Medical Journal 314:25,1997
12. Zolghadri, B.Gharesi. The Prevalence of Antiphospholipid Syndrome in patients with recurrent pregnancy loss: A report from South Iran. MJIRI, Vol.18, No.2,119-121,2004.
13. Gharavi AE, Harris EN, Asherson RA, Hughes GR. Anticardiolipin antibodies: isotype distribution and phospholipid specificity. Ann Rheum Dis. 1987 Jan;46(1):1-6.
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

