The Utility of Plasma Transthyretin and Antioxidants as aBiomarker of Early Pregnancy Loss - A Pilot Study
Abstract
Objective: Miscarriage or early pregnancy loss (EPL) affects about 15-25% of all pregnancies and is considered as one of the most common complications of the human reproduction. The objective of this pilot study was to quantify and compare the levels of plasma Transthyretin (TTR) and total antioxidant capacity (TAC)among EPL patients and normal pregnant women.
Design: Cross sectional pilot study.
Subjects: Patients diagnosed with EPL in their first trimester (Incomplete and Missed abortion) and medically terminated pregnancy (MTP) and pregnant women in their first trimester of pregnancy without any complications.
Methods: Plasma TTR and total antioxidantcapacity were quantified using Enzyme Linked Immunosorbent Assay (ELISA) and Trolox equivalent antioxidant capacity assay respectively. Statistical analyses were performed with SPSS software version 16.0 (SPSS Inc., Chicago, IL). All p values <0.05 were considered statisticallysignificant.
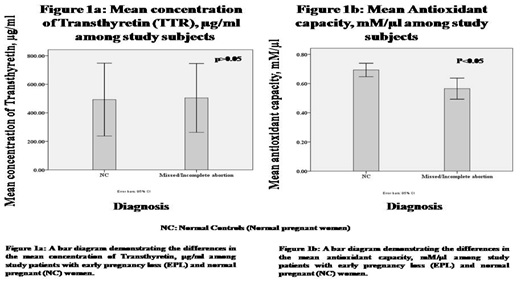
Results:A total of 60 subjects were enrolled in the study. There was no significant difference in the mean concentration of plasma TTR among women with EPL 322.20(187.33-444.10) µg/ml and normal pregnant women 224.32(176.06-509.97) µg/ml (p=0.501). However, a significant difference was observed in the TACamong women with EPL 0.58 (0.51-0.70) mM/μl and normal pregnant women 0.71 (0.63-0.79) mM/μl (p=0.006). No significant correlation was seen between TTR and antioxidant capacity.
Conclusion: Our study failed to demonstrate any relationship between plasma TTR levels and EPL. Antioxidant capacity was lower among EPL patients suggesting the importance of supplementation with antioxidants to prevent poor outcomes in pregnancy.
Downloads
References
2. Jauniaux E, Burton GJ. Pathophysiology of histological changes in early pregnancy loss. Placenta. 2005 Feb-Mar;26(2-3):114-23.[pubmed]
3. Haddow JE, Palomaki GE, Allan WC, et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N Engl J Med. 1999 Aug 19;341(8):549-55.[pubmed]
4. Landers KA, McKinnon BD, Li Het al. Carrier-mediated thyroid hormone transport into placenta by placental transthyretin. J Clin Endocrinol Metab. 2009 Jul;94(7):2610-6. doi: 10.1210/jc.2009-0048. Epub 2009 Apr 28.
5. Fleming CE, Nunes AF, Sousa MM. Transthyretin: more than meets the eye. Prog Neurobiol. 2009 Nov;89(3):266-76. doi: 10.1016/j.pneurobio.2009.07.007. Epub 2009 Aug 7.[pubmed]
6. Landers KA, Mortimer RH, Richard K. Transthyretin and the human placenta. Placenta. 2013 Jul;34(7):513-7. doi: 10.1016/j.placenta.2013.04.013. Epub 2013 May 9.[pubmed]
7. Fruscalzo A, Schmitz R, Klockenbusch W, Köhler G, Londero AP, Siwetz M, et al. Human placental transthyretin in fetal growth restriction in combination with preeclampsia and the HELLP syndrome. Histochem Cell Biol. 2012 Dec;138(6):925–32.doi: 10.1007/s00418-012-0997-1. Epub 2012 Jul 31.[pubmed]
8. Wang Q, Liu C, Zhang Z. Transthyretin and Normal Human Pregnancy: Mini Review. Crit Rev Eukaryot Gene Expr. 2016;26(3):273-7. doi: 10.1615/CritRevEukaryotGeneExpr.2016017323.[pubmed]
9. Fruscalzo A, Biasioli A, Londero AP, Ceraudo M, Stel G, Bertozzi S, et al. Retinol binding protein as early marker of fetal growth restriction in first trimester maternal serum. Gynecol Endocrinol Off J Int Soc Gynecol Endocrinol. 2013 Apr;29(4):323–6.doi: 10.3109/09513590.2012.743013. Epub 2013 Jan 25.
10. Mistry HD, Gill CA, Kurlak LO, et al. Association between maternal micronutrient status, oxidative stress, and common genetic variants in antioxidant enzymes at 15 weeks׳ gestation in nulliparous women who subsequently develop preeclampsia. Free Radic Biol Med. 2015 Jan;78:147-55. doi: 10.1016/j.freeradbiomed.2014.10.580. Epub 2014 Nov 6.[pubmed]
11. Zhu L, Chen Y, Liu C, et al. Transthyretin as a novel candidate biomarker for preeclampsia. Exp Ther Med. 2014 May;7(5):1332-1336. Epub 2014 Feb 18.[pubmed]
12. Vascotto C, Salzano AM, D'Ambrosio C, et al. Oxidized transthyretin in amniotic fluid as an early marker of preeclampsia. J Proteome Res. 2007 Jan;6(1):160-70.[pubmed]
13. Liu AX, Jin F, Zhang WW, et al. Proteomic analysis on the alteration of protein expression in the placental villous tissue of early pregnancy loss. Biol Reprod. 2006 Sep;75(3):414-20. Epub 2006 May 31.[pubmed]
14. Episkopou V, Maeda S, Nishiguchi S, et al. Disruption of the transthyretin gene results in mice with depressed levels of plasma retinol and thyroid hormone. Proc Natl Acad Sci U S A. 1993 Mar 15;90(6):2375-9.[pubmed]
15. Divino CM, Schussler GC. Receptor-mediated uptake and internalization of transthyretin. J Biol Chem. 1990 Jan 25;265(3):1425-9.[pubmed]
16. Sousa MM, Saraiva MJ. Internalization of transthyretin. Evidence of a novel yet unidentified receptor-associated protein (RAP)-sensitive receptor. J Biol Chem. 2001 Apr 27;276(17):14420-5. Epub 2001 Jan 24.[pubmed]
17. Hussain M, El-Hakim S, Cahill DJ. Progesterone supplementation in women with otherwise unexplained recurrent miscarriages. J Hum Reprod Sci. 2012 Sep;5(3):248-51. doi: 10.4103/0974-1208.106335.[pubmed]
18. Lepoutre T, Debiève F, Gruson D, et al. Reduction of miscarriages through universal screening and treatment of thyroid autoimmune diseases. GynecolObstet Invest. 2012;74(4):265-73. doi: 10.1159/000343759. Epub 2012 Nov 10.[pubmed]
19. Omeljaniuk WJ, Socha K, Borawska MH, et al. Antioxidant status in women who have had a miscarriage. Adv Med Sci. 2015 Sep;60(2):329-34. doi: 10.1016/j.advms.2015.06.003. Epub 2015 Jul 5.[pubmed]
20. Jenkins C, Wilson R, Roberts J, et al. Antioxidants: their role in pregnancy and miscarriage. Antioxid Redox Signal. 2000 Fall;2(3):623-8. DOI:10.1089/15230860050192369
21. Poston L, Raijmakers MT. Trophoblast oxidative stress, antioxidants and pregnancy outcome--a review. Placenta. 2004 Apr;25 Suppl A:S72-8.[pubmed]
22. Poston L, Igosheva N, Mistry HD, et al. Role of oxidative stress and antioxidant supplementation in pregnancy disorders. Am J Clin Nutr. 2011 Dec;94(6 Suppl):1980S-1985S. doi: 10.3945/ajcn.110.001156. Epub 2011 May 25.[pubmed]
23. Baban RS. Oxidative stress in recurrent pregnancy loss women. Saudi Med J. 2010 Jul;31(7):759-63.[pubmed]
24. Yiyenoğlu ÖB, Uğur MG, Özcan HÇ, et al. Assessment of oxidative stress markers in recurrent pregnancy loss: a prospective study. Arch Gynecol Obstet. 2014 Jun;289(6):1337-40. doi: 10.1007/s00404-013-3113-4. Epub 2013 Dec 3.[pubmed]
25. Simşek M, Naziroğlu M, Simşek H, et al. Blood plasma levels of lipoperoxides, glutathione peroxidase, beta carotene, vitamin A and E in women with habitual abortion. Cell BiochemFunct. 1998 Dec;16(4):227-31.[pubmed]
26. Patel J, Landers KA, Li H, et al. Ontogenic changes in placental transthyretin. Placenta. 2011 Nov;32(11):817-22. doi: 10.1016/j.placenta.2011.09.007. Epub 2011 Sep 25.
27. Schneider H. Oxygenation of the placental-fetal unit in humans. Respir PhysiolNeurobiol. 2011 Aug 31;178(1):51-8. doi: 10.1016/j.resp.2011.05.009. Epub 2011 May 17.[pubmed]
28. Patel J, Landers K, Mortimer RH, et al. Regulation of hypoxia inducible factors (HIF) in hypoxia and normoxia during placental development. Placenta. 2010 Nov;31(11):951-7. doi: 10.1016/j.placenta.2010.08.008. Epub 2010 Sep 24.[pubmed]
29. Patel J, Landers K, Li H, et al. Oxygen concentration regulates expression and uptake of transthyretin, a thyroxine binding protein, in JEG-3 choriocarcinoma cells. Placenta. 2011 Feb;32(2):128-33. doi: 10.1016/j.placenta.2010.11.016. Epub 2010 Dec 10.
Copyright (c) 2019 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

