Husband’s participation in birth preparedness and complication readiness
Abstract
Introduction: Pregnancy and childbirth continue to be viewed as solely a woman’s issue. Finding a male companion at antenatal care is rare. Husbands in patriarchal societies of developing countries are often identified as decision makers in all aspects of day-to-day life. Thus Husband’s participation promotes active preparation and assists in decision-making in birth preparedness and in case of complications.
Aim: The main objective of this study was to assess the determinant factors of male involvement in birth preparedness and complication readiness.
Materials and Methods: A cross-sectional survey was conducted among 100 married Couples from June 2018 to October 2018 in tertiary care hospital, Adichunchangiri Institute of Medical Sciences, B.G Nagara, Karnataka. Data collected Using pre-structured questionnaire, Odds Ratio and 95% confidence interval.
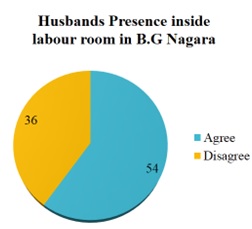
Results: A total of 100 husbands participated in the study with 95% response rate. About 70% of the husbands had participated in birth preparedness and complication readiness. The study revealed that husbands were more likely to participate in birth preparedness if they had better knowledge in postnatal danger signs and a better knowledge on birth preparedness.
Conclusion: Educated and Young aged Husbands with higher income and formal employment showed greater involvement in birth preparedness and complication readiness. Hence these factors should be emphatically considered during maternal health program development. Male awareness in postnatal danger signs and birth preparedness should be increased by local and other concerned bodies.
Downloads
References
2. United Nations Population Fund: A new role for men: Partners for Women’s Empowerment. 1997, NY: UNFPA.
3. United Nation Population Fund; SI and Burger, M.: Parentinga new approach to sexual and reproductive health. Technical paper No.3, 2000.
4. Federal Democratic Republic of Ethiopian. Ministry of Health: Antenatal Care Blended learning module for the Health extension Programmme, HEAT in Africa.
5. JHPIEGO: Maternal and Neonatal health (MNH) program, birth preparedness and complication readiness: A matrix of shared responsibilities. Maternal and Neonatal Health. 2001, 23-31.Google Scholar
6. Hiluf M, Fantahun M: Birth Preparedness and Complication Readiness among women in Adigrat town, north Ethiopia. Ethiop J Health Dev 2007, 22(1):14–20.
7. Federal democratic republic of Ethiopia ministry of health, basic emergency obstetric & newborn care (BEMONC) training manual. A: Ministry of health, April 2010,1st Ed.
8. McPherson RA, Khadka N, Moore JM, Sharma M: Are birth-preparedness programmes effective? Results from a field trial in Siraha district, Nepal. Journal of Health Population and Nutrition. 2006, 24 (4): 479-88.Google Scholar
9. Babalola S, Fatusi A: Determinants of use of maternal health services in Nigeria–looking beyond individual and household factors. BMC Pregnancy & Childbirth. 2009, 9: 43-10.1186/1471-2393-9-43.View ArticleGoogle Scholar
10. United Nations. The sustainable development goals report 2016. 2016.Google Scholar
11. Katz DA, Kiarie JN, John-Stewart GC, et al. Male perspectives on incorporating men into antenatal HIV counseling and testing. PLoS One. 2009 Nov 2;4(11):e7602. doi: 10.1371/journal.pone.0007602.[pubmed]
12. Iliyasu Z, Abubakar IS, Galadanci HS, et al. Birth preparedness, complication readiness and fathers' participation in maternity care in a northern Nigerian community. Afr J Reprod Health. 2010 Mar;14(1):21-32.[pubmed]
13. Odimegwu C, Adewuyi A, Odebiyi T, et al. Men's role in emergency obstetric care in Osun State of Nigeria. Afr J Reprod Health. 2005 Dec;9(3):59-71.[pubmed]
14. Katz DA, Kiarie JN, John-Stewart GC, et al. Male perspectives on incorporating men into antenatal HIV counseling and testing. PLoS One. 2009 Nov 2;4(11):e7602. doi: 10.1371/journal.pone.0007602.[pubmed]
15. Msuya SE, Mbizvo EM, Hussain A, et al. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: implications for preventive programs. AIDS Care. 2008 Jul;20(6):700-9. doi: 10.1080/09540120701687059.[pubmed]
16. Martin LT, McNamara MJ, Milot AS, Halle T, Hair EC: The effectsOrne-Gliema involvement during pregnancy on receipt of prenatal care and maternal smoking. Maternal Child Health J. 2007, 11: 595-602. 10.1007/s10995-007-0209-0.View ArticlePubMedGoogle Scholar
17. Orne-Gliemann J, Desgrées-Du-Loû A. The involvement of men within prenatal HIV counselling and testing. Facts, constraints and hopes. AIDS. 2008 Nov 30;22(18):2555-7. doi: 10.1097/QAD.0b013e32831c54d5.[pubmed]
18. Onayade AA, Akanbi OO, Okunola HA, et al. Birth preparedness and emergency readiness plans of antenatal clinic attendees in Ile-ife, Nigeria. Niger Postgrad Med J. 2010 Mar;17(1):30-9.[pubmed]
19. Mutiso SM, Qureshi Z, Kinuthia J. Birth preparedness among antenatal clients. East Afr Med J. 2008 Jun;85(6):275-83.[pubmed]
20. World Health Organization. WHO recommendations on health promotion interventions for maternal and newborn health 2015: World Health Organization; 2015.Google S
21. Biza A, Jille-Traas I, Colomar M, et al. Challenges and opportunities for implementing evidence-based antenatal care in Mozambique: a qualitative study. BMC Pregnancy Childbirth. 2015 Sep 2;15:200. doi: 10.1186/s12884-015-0625-x.[pubmed]
22. August F, Pembe AB, Mpembeni R, Axemo P, Darj E. Men’s knowledge of obstetric danger 23]signs, birth preparedness and complication readiness in rural Tanzania. PLoS One.[pubmed]
22. August F, Pembe AB, Mpembeni R, et al. Men's Knowledge of Obstetric Danger Signs, Birth Preparedness and Complication Readiness in Rural Tanzania. PLoS One. 2015 May 7;10(5):e0125978. doi: 10.1371/journal.pone.0125978. eCollection 2015.
23. Kabakyenga JK, Östergren PO, Turyakira E, et al. Influence of birth preparedness, decision-making on location of birth and assistance by skilled birth attendants among women in south-western Uganda. PLoS One. 2012;7(4):e35747. doi: 10.1371/journal.pone.0035747. Epub 2012 Apr 27.[pubmed]
24. Wai KM, Shibanuma A, Oo NN, Fillman TJ, Saw YM, Jimba M. Are husbands involving in their spouses’ utilization of maternal care services?: a cross-sectional study in Yangon, Myanmar. PLoS One. 2015;10(12):e0144135.View ArticlePubMedPubMedCentralGoogle Scholar
25. Iliyasu Z, Abubakar IS, Galadanci HS, et al. Birth preparedness, complication readiness and fathers' participation in maternity care in a northern Nigerian community. Afr J Reprod Health. 2010 Mar;14(1):21-32.[pubmed]
26. Haftom Gebrehiwot Weldearegay. Determinant Factors of Male Involvement in Birth Preparedness and Complication Readiness at MekelleTown; a community Based Study. Science Journal of Public Health. Vol. 3, No. 2, 2015, pp. 175-180. doi: 10.11648/j.sjph.20150302.14.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

