Prevalence of hypothyroidism in pregnancy
Abstract
Introduction: Pregnancy is a period that places great physiological stress on both the mother and the fetus. Thyroid disorders are among the common endocrine disorders in pregnant women after diabetes mellitus. Several changes are observed in maternal thyroid function during pregnancy and failure to adapt to these physiological changes results in thyroid dysfunction. When pregnancy is compounded by endocrine disorders such as hypothyroidism, the potential for maternal and fetal adverse outcomes can be immense.
Methods: The present study was conducted at KIMS hospital, Narketpally. It is a prospective type of study which includes 48 patients diagnosed to have thyroid disorder during their antenatal checkup in the first trimester. It also includes known cases of thyroid disorder. TSH level was estimated. If it is deranged, then FT3 and FT4 levels were estimated. Prevalence of hypothyroidism was noted. Patients were managed accordingly and followed till delivery. Their obstetric and perinatal outcomes were noted.
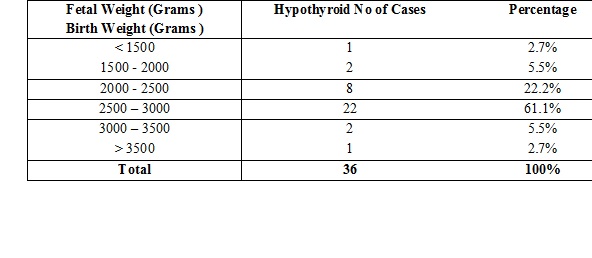
Results: In the present study, 48 out of 700 pregnant women screened had thyroid disorders. The prevalence of Hypothyroidism in this study is 6.8%.In the present study, it is affecting more in the age group of 21 to 30 yrs in multigravida, the prevalence of subclinical hypothyroidism is 6.1% and overt hypothyroidism is 0.7% .86% of pregnancies with SCH had cesarean section, fetal distress (48.38%) being the most common indication. The perinatal mortality rate in hypothyroid women was found out to be 5.5%.
Conclusion: Routine screening, early confirmation of diagnosis and prompt treatment is required to ensure favorable maternal and fetal outcomes. Subclinical hypothyroidism also needs to be detected and treated to prevent adverse outcomes. It is difficult to diagnose hypothyroidism clinically in pregnancy due to non specific presenting features which may be masked by existing obstetric symptoms. While targeted case finding is generally practiced, recent evidence seems to indicate that universal screening might be a better option.
Downloads
References
2. Klein RZ, Haddow JE, Faix JD, et al. Prevalence of thyroid deficiency in pregnant women. Clin Endocrinol (Oxf). 1991 Jul;35(1):41-6.[pubmed]
3. Mandel SJ. Hypothyroidism and chronic autoimmune thyroiditis in the pregnant state: maternal aspects. Best Pract Res Clin Endocrinol Metab. 2004 Jun;18(2):213-24. DOI:10.1016/j.beem.2004.03.006
4. Goel P, Radotra A, Devi K, et al. Maternal and perinatal outcome in pregnancy with hypothyroidism. Indian J Med Sci. 2005 Mar;59(3):116-7.[pubmed]
5. Amino N, Izumi Y, Hidaka Y, No increase of blocking type anti-thyrotropin receptor antibodies during pregnancy in patients with Graves' disease. J Clin Endocrinol Metab. 2003 Dec;88(12):5871-4.[pubmed]
6. LeBeau SO, Mandel SJ. Thyroid disorders during pregnancy. Endocrinology and Metabolism Clinics of North America, 2006; 35(1): 117–136.[pubmed]
7. Amino N, Tada H, Hidaka Y, et al. Postpartum autoimmune thyroid syndrome. Endocr J. 2000 Dec;47(6):645-55.[pubmed]
8. Sahu MT et al. Overt and subclinical thyroid dysfunction among Indian pregnant women and its effect on maternal and fetal outcome. Archives of gynecology and obstetrics. 2010;281(2):215-220.[pubmed]
9. Dhanwal DK, Prasad S, Agarwal AK, et al. High prevalence of subclinical hypothyroidism during first trimester of pregnancy in North India. Indian J Endocrinol Metab. 2013 Mar;17(2):281-4. doi: 10.4103/2230-8210.109712.[pubmed]
10. Marwaha RK, Tandon N, Gupta N, et al. Residual goitre in the postiodization phase: iodine status, thiocyanate exposure and autoimmunity.Clin Endocrinol (Oxf). 2003 Dec;59(6):672-81.[pubmed]
11. Teng X, Shan Z, Chen Y, et al. More than adequate iodine intake may increase subclinical hypothyroidism and autoimmune thyroiditis: a cross-sectional study based on two Chinese communities with different iodine intake levels. Eur J Endocrinol. 2011 Jun;164(6):943-50. doi: 10.1530/EJE-10-1041. Epub 2011 Mar 28.[pubmed]
12. Das S, Bhansali A, Dutta P, Aggarwal A, Bansal MP, Garg D, et al. Persistence of goitre in the post-iodization phase: Micronutrient deficiency or thyroid autoimmunity? Indian J Med Res. 2011;133:103–9.[pubmed]
13. Gayathri R, Lavanya S, Raghavan K. Subclinical hypothyroidism and autoimmune thyroiditis in pregnancy--a study in south Indian subjects. J Assoc Physicians India. 2009 Oct;57:691-3.[pubmed]
14. Unnikrishnan AG, Kalra S, Sahay RK, Prevalence of hypothyroidism in adults: An epidemiological study in eight cities of India. Indian J Endocrinol Metab. 2013 Jul;17(4):647-52. doi: 10.4103/2230-8210.113755.[pubmed]
15. Joshi K, Bhatt M, Saxena R. Incidence of thyroid dysfunction in antenatal women and its effect on fetomaternal outcome. IAIM, 2016; 3(11): 136-142.
16. Aziz Nuzhat, Reddy Pranathi, Fernandez Evita. Hypothyroidism in pregnancy: Is universal screening needed? Journal of Obstetrics and Gynecology of India 2006;56(6).
17. Vaidya B, Anthony S, Bilous M, et al. Detection of thyroid dysfunction in early pregnancy: Universal screening or targeted high-risk case finding? J Clin Endocrinol Metab. 2007 Jan;92(1):203-7. Epub 2006 Oct 10. DOI:10.1210/jc.2006-1748.
Copyright (c) 2018 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

