The Obstetric Risk and Neonatal Consequences of Adolescent Pregnancy
Abstract
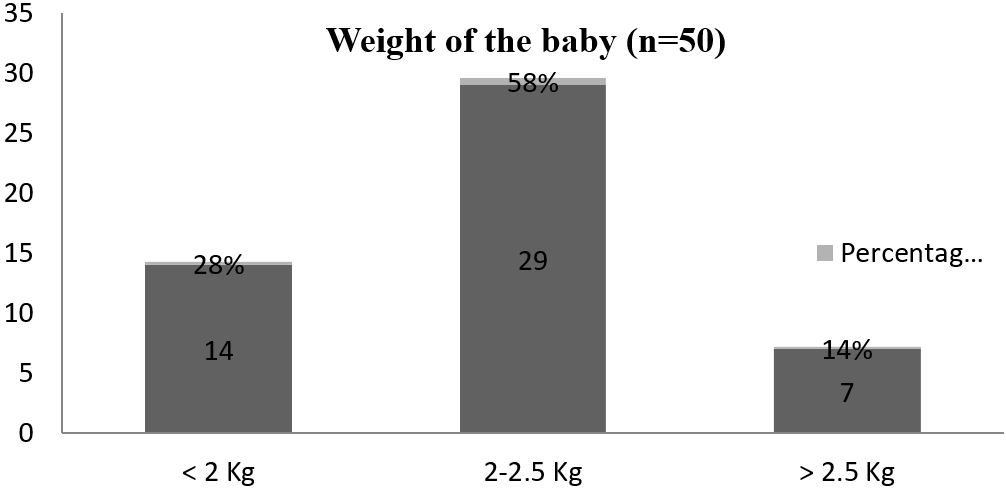
Introduction: Adolescent pregnancy is a worldwide problem bearing serious social and medical implications relating to maternal and child health. Adolescent pregnancy is a complex and frustrating problem of both developed and developing countries. Methods: A Cross-sectional observational study was carried out in the Department of Department of obstetrics and gynecology; Dhaka medical college & hospital, Dhaka, a tertiary level of hospital of Bangladesh from 1st July 2015 – 31st December 2015. 50 patients presented with adolescent pregnancy (Primigravida without medical complications) diagnosed on clinical, biochemical, investigational background were enrolled in the study, fulfilling the inclusion and exclusion criteria. Results; It revealed that the maximum number of teenage patients 44(88%) were between the age group of 17 to 19 years. The present study showed that majority of teenage mothers were Muslim 43(86%). Most of the teenage mothers were housewives 42(84%), then garments worker 4(8%), then day labourer 2(4%), maid servants 1(2%), student 1(2%). Study also showed that 68% of teenage mothers belong to the monthly income group below TK. 3000; in other words most of the teenage mothers had come from a low socioeconomic class. Clinical examination findings showed 25(50%) of teenage mothers were anaemic, 10(20%) had oedema, 8(16%) were hypertensive. Among the antepartum and intrapartum complication, current study shows maximum number of patients 25(50%) were affected with anemia and 17(34%) teenage mother developed no complication. Current study also showed that APGAR score of the baby at first minute 27(54%) were greater than 7 and 23(46%) were less than 7. Maximum number of babies 29(58%) were between 2-2.5 kg, 14(28%) were very low birth weight and only 7(14%) of baby birth weight greater than 2.5 kg. Study showed 14(28%) of the babies developed birth asphyxia, 8(16%) had prematurity, 2(4%) had jaundice. Conclusion: We observed low birth weight is a key predictor for fetal complication and child mortality. It may be due to babies born to adolescent mothers are likely to be premature, and hence, the incidence of low birth weight is higher in them.
Downloads
References
2. Bangladesh Demographic and Health Survey (BDHS)-2011.
3. Kumar P, Malhotra N. Jeffcoate's Principles of Gynaecology; (Revised and updated), 7th edition, Arnold, 2008; 6:111-114.
4. Agarwal N, Reddaiah VP. Factors affecting birthweight in a suburban community. Health Popul Perspect Issue.2005;28:189–96.
5. World Health Organization. Towards adulthood: exploring the sexual and reproductive health of adolescents in South Asia.Geneva: World Health Organization; 2003. p. 244.
6. Jeffcoate N. Jeffcoate's principle of gynecology, 6th edition, published by Arnold 2001:5,90, 20-59.
7. Population reports, Youth in 1980, Series M.November–December 1985.
8. Rao KB, Perinatal mortality. In Ratnam SS, Rao KE Arul Kumaran S Ec-tors, obstetrics and qynaecology for post graduates, vol.-Ki-2 1st edition (252-12).
9. Halida Hanum Akhter, M. Hafizur Rahman and Famida Karim. A study of identify the risk factors affecting nutritional status of adolescent girls in Bangladesh. B1RPERHT, Dhaka, December 1998, IX.
10. SS Ratnam, K Bhaskor Rao, S Arul Kumaran.obstetrics and gynecology. Vol – 21st edition, Orient Longman limited, 1999:23.287.
11. SS Ratnam, K. Bhaskor Roy, S Arul Kumaran. Obstetrics and Gynaecology, Vol.12th edition, Orient Longman limited, 1999;1:2-4.
12. Prianka Mukhopadhyay, R.N. Chaudhuri and Bhaskar Paul “Hospital-based Perinatal Outcomes and Complications in Teenage Pregnancy in India". Journal of Health, Population, and Nutrition. Oct 2010; 28(5): 494-500.
13. Haider SJ. Saleh SN, Kamal N. Study of adolescent's dynamics of perception Attitude knowledge and use of reproductive health care Population council (1995).
14. Ghose N Ghosh B. Obstetrics behavior in teenagers (a study of 1138 consecutive Cases), journal of obstetrics & Gynecology India 1976, 26:722–26.
15. Sakar CS, Giri AK, Sarkar B; Outcome of teenage pregnancy and labour. Journal of Indian Med Assoc, 1991 89(7), 197-9.
16. Cooksey EC, Rindfuss RR, Guilkey DK, The initiation of adolescent sexual and Contraceptive behavior during changing times. J Health Soc Behav 1996, 37;59-74.
17. BAMBEIS Report 2012.
18. World Health Organization. Adolescent pregnancy: issues in adolescent health and development. Geneva: World Health Organization; 2004, p. 86. (WHO discussion papers on adolescence).
19. Verma V, Das KB. Teenage primigravida: a comparative study. Indian J Public Health. 1997:41:52–5.
20. Cahaba S. Perinatal outcome in teenage mothers. J Obstet Gynaecol India. 1991:41:30–2.
21. Pal A, Gupta KB, Randhawal. Adolescent pregnancy: a high risk group. J Indian Med Assoc. 1997;95:127–8.
22. Sharma AK, Verma K, Khatri S, Kannan AT. Pregnancy in adolescents: study of risks and outcome in eastern Nepal. Indian Pediatr. 2001;38:1405–9.
23. Nayak AH, Purnik KG, Dalal AR. Obstetric outcome in teenage pregnancy. J Obstet Gynecol India. 1992;42:442–6.
24. Pregnancy and Labour in young girls by Porozhanova V Bozhinova S-sa Kuss Genekel (Sufiia) 1994,33(3): 15-7.
25. Fraser AM, Brockert JE, Ward RH. Association of young maternal age with adverse reproductive outcomes. N Engl J Med. 1995;332:1113–7.
26. Adam GK, Elhassan EM, Ahmed AM, Adam I. Maternal and perinatal outcome in teenage pregnancies in Sudan. Int J Gynaecol Obstet. 2009;105:170–1.
27. Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol. 2007:36:368–73.
28. Buitendijk SE, van Enk A, Oosterhout R, Ris M. [Obs-tetrical outcome in teenage pregnancies in The Netherlands] Ned Tijdschr Geneeskd. 1993, 137:2536-40.
29. Ali M. Lulseged S. Factors influencing adolescent birth outcome. Ethiop med J 1997:35:35-42.
30. Kushwaha KP, Rai AK, Rathi AK, Singh YD, Sirohi R. Pregnancies in adolescents: fetal, neonatal and maternal outcome. Indian Pediatr. 1993;30:501–5.
31. Mehra S, Agrawal D. Adolescent health determinants for pregnancy and child health outcomes among the urban poor.Indian Paediatr. 2004;41:137–45.
32. Gortzak-Uzan L, Hallak M, Press F, Katz M, Shoham-Vardi I. Teenage pregnancy: risk factors for adverse perinatal outcome. J Matern Fetal Med. 2001;10:393–7.
33. Sharma V, Katz J, Mullany LC, Khatry SK, LeClerq SC, Shrestha SR, et al. Young maternal age and the risk of neonatal mortality in rural Nepal. Arch Pediatr Adolesc Med.2008;162:828-35.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

