Study Of Fetomaternal Outcome In Cases Of Placenta Previa At Tertiary Care Hospital, Dhaka, Bangladesh
Abstract
Background: Placenta previa remains a significant obstetric challenge associated with substantial maternal and fetal morbidity. The increasing incidence of placenta previa and its associated complications, particularly in the context of rising cesarean section rates, necessitates ongoing evaluation of management strategies and outcomes.
Objective: To assess the fetomaternal outcomes in cases of placenta previa managed at a tertiary care hospital and to identify risk factors associated with adverse outcomes.
Methods:This retrospective observational study analyzed 60 cases of placenta previa managed at FetomaternalMedicine Dept., BSMMU, Dhaka, Bangladesh between June 2023 to June 2024.Data on maternal characteristics, obstetric factors, management strategies, and fetomaternal outcomes were collected from medical records. Statistical analysis included descriptive statistics and multivariate logistic regression to identify risk factors for adverse outcomes.
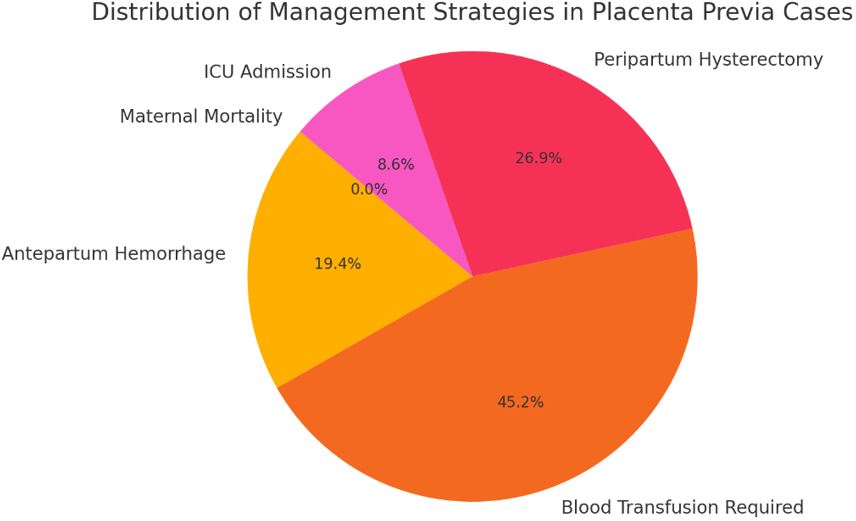
Results: The mean maternal age was 29.2 ± 4.3 years, with 75% of patients having a history of previous cesarean sections. Placenta previa was diagnosed in 76.7% of cases, andlow lying placenta were present in 23.3%. Peripartum hysterectomy was performed in 41.7% of cases. The preterm delivery rate was 70%, with a mean gestational age at delivery of 35.6 ± 2.8 weeks. Neonatal intensive care unit admission was required for 36.7% of newborns, and the perinatal mortality rate was 3.3%. Multivariate analysis identified previous cesarean sections (≥2) (adjusted OR 3.8, 95% CI 1.7-8.5) and placenta accreta spectrum disorders (adjusted OR 12.5, 95% CI 4.2-37.1) as significant risk factors for peripartum hysterectomy.
Conclusion: This study highlights the significant maternal and fetal morbidity associated with placenta previa, particularly in cases with previous cesarean sections and placenta accreta spectrum disorders. The findings underscore the importance of early diagnosis, multidisciplinary management, and the need for specialized care in tertiary centers for high-risk pregnancies. Strategies to reduce primary cesarean section rates and careful counseling for women with a history of cesarean delivery are crucial in addressing this growing obstetric challenge.
Downloads
References
2. Silver RM. Abnormal Placentation: Placenta Previa, Vasa Previa, and Placenta Accreta. Obstet Gynecol. 2015;126(3):654-668.
3. Ananth CV, Smulian JC, Vintzileos AM. The effect of placenta previa on neonatal mortality: a population-based study in the United States, 1989 through 1997. Am J Obstet Gynecol. 2003;188(5):1299-1304.
4. Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005;192(5):1458-1461.
5. Crane JM, Van den Hof MC, Dodds L, Armson BA, Liston R. Maternal complications with placenta previa. Am J Perinatol. 2000;17(2):101-105.
6. Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107(6):1226-1232.
7. Shamshirsaz AA, Fox KA, Salmanian B, et al. Maternal morbidity in patients with morbidly adherent placenta treated with and without a standardized multidisciplinary approach. Am J Obstet Gynecol. 2015;212(2):218.e1-218.e9.
8. Eller AG, Bennett MA, Sharshiner M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011;117(2 Pt 1):331-337.
9. Vahanian SA, Lavery JA, Ananth CV, Vintzileos A. Placental implantation abnormalities and risk of preterm delivery: a systematic review and metaanalysis. Am J Obstet Gynecol. 2015;213(4 Suppl):S78-S90.
10. Nørgaard LN, Pinborg A, Lidegaard Ø, Bergholt T. A Danish national cohort study on neonatal outcome in singleton pregnancies with placenta previa. ActaObstetGynecol Scand. 2012;91(5):546-551.
11. Balayla J, Wo BL, Bédard MJ. A late-preterm, early-term stratified analysis of neonatal outcomes by gestational age in placenta previa: defining the optimal timing for delivery. J Matern Fetal Neonatal Med. 2015;28(15):1756-1761.
12. Pilloni E, Alemanno MG, Gaglioti P, et al. Accuracy of ultrasound in antenatal diagnosis of placental attachment disorders. Ultrasound Obstet Gynecol. 2016;47(3):302-307.
13. Bowman ZS, Eller AG, Kennedy AM, et al. Accuracy of ultrasound for the prediction of placenta accreta. Am J Obstet Gynecol. 2014;211(2):177.e1-177.e7.
14. Baba Y, Matsubara S, Ohkuchi A, et al. Anterior placentation as a risk factor for massive hemorrhage during cesarean section in patients with placenta previa. J ObstetGynaecol Res. 2014;40(5):1243-1248.
15. Kassem GA, Alzahrani AK. Maternal and neonatal outcomes of placenta previa and placenta accreta: three years of experience with a two-consultant approach. Int J Womens Health. 2013;5:803-810.
16. Tikkanen M, Stefanovic V, Paavonen J. Placenta previapercreta left in situ - management by delayed hysterectomy: a case report. J Med Case Rep. 2011;5:418.
17. Sentilhes L, Ambroselli C, Kayem G, et al. Maternal outcome after conservative treatment of placenta accreta. Obstet Gynecol. 2010;115(3):526-534.
18. Jauniaux E, Bhide A. Prenatal ultrasound diagnosis and outcome of placenta previa accreta after cesarean delivery: a systematic review and meta-analysis. Am J Obstet Gynecol. 2017;217(1):27-36.
19. Melcer Y, Jauniaux E, Maymon S, et al. Impact of targeted scanning protocols on perinatal outcomes in pregnancies at risk of placenta accreta spectrum or vasa previa. Am J Obstet Gynecol. 2018;218(4):443.e1-443.e8.
20. Gyamfi-Bannerman C, Srinivas SK, Wright JD, et al. Postpartum hemorrhage outcomes and race. Am J Obstet Gynecol. 2018;219(2):185.e1-185.e10.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

