Evaluation of Pregnancy Outcome in Severe Preeclampsia
Abstract
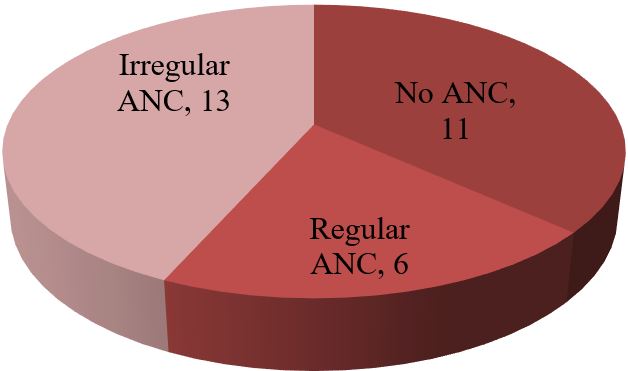
Background: Hypertensive disorder represent the most common medical complication of pregnancy affecting between 7 to 15 percent of all gestation and account for approximately a quarter of all antenatal admission. In Bangladesh the incidence of this killer disease is still high and it is third major cause of maternal death in our country. Objective: To evaluate pregnancy outcome in severe preeclampsia. Study design: Observational cross sectional study. Place of study: In Obstetrics & Gynaecology ward of BSMMU, Dhaka. Period of study: March, 2015 to August, 2015. Sample size: 30 patients were selected by purposive sampling. Methods: The data were collected by the active participation of the patients' interview by the preformed proforma of data collection sheet and then data were gathered, decorated, tabulated after data cleaning and edition. Then the results were found and they were tested by the student's unpaired t test (quantitative data) and chi-square test (qualitative data) to see their level of significance i,e p-value which was set as the cut off level at <0.05. So if p-value is >0.05 the results are no significant.Results: The mean age of 30 mothers were 27.65 (± 5.85) years. The maximum 19 (63.33%) patients were from 20-34 years age group. Among the 30 mothers with severe preeclampsia, 12(40%) were primiparous and rest 18 (60%) were multiparous. To ensure safe delivery 14(46.67%) mothers adopted LSCS whereas 10(33.33%) adopted vaginal delivery with episiotomy. The rest 6 (20%) underwent VD. Regular ANC ensured only 6 (20%) respondents whereas rest 80% replied that they were either irregular ANC or no ANC. The most common complications mothers faced was abruptio placenta (28.57%) followed by convulsion (14.28%) and HELLP syndrome (9.52%). Amo. Neonatal mortality was found in 4 cases out of 30. 60% neonate experienced low birth weight. 45% babies required neonatal ward admission whereas 62% required resuscitation. Conclusion: In conclusion, it may be assumed that though various fetal and maternal morbidities may occur in case of severe preeclampsia but mortality is seen only in case of neonates. Maternal mortality has been almost disappeared in our perspective in case of severe pre-eclampsia.
Downloads
References
2. Mashiloane CD, Moodley J. Induction or Caesarean section for pre-term preeclampsia. Journal of Obstetrics and Gynecology 2002; 22(4): 353-356.
3. Duley L. Maternal mortality associated with hypertensive disorders of pregnancy in Africa, Asia, Latin America and the Caribbean. Br J ObstetGynaecol. 1992; 99(7): 547-53.
4. Statistics by country for preeclampsia: extrapolation of incidence rate for preeclampsia tocountries and regions. Available from: http://www.wrongdiagnosis.com/p/preeclampsia/stats-country. htm [accessed on 15th April, 2010].
5. Dutta DC. Hypertensive disorders in pregnancy. In: Text book of obstetrics including perinatology and contraception. 6th ed. Calcutta: New Central Book Agency; 2004; 221-42.
6. Bangladesh demographic and health survey: summary indicators. National Institute of Population Research and Training (NIPORT), Dhaka, Bangladesh. 2005.
7. Viswanathan M, Daniel S.The study of maternal outcome of early onset severe pre-eclampsia with expectant management. Int J. ReprodContraceptObstet Gynecol. 2014;3(1):92-97.
8. MattarF,Sibai BM: Eclampsia viii riskfactors for maternal morbidity. Am J Obstet Gynecol. 2000; 182:307-312.
9. Brown MA, Buddle ML Hypertension in Pregnancy: Maternal and neonatal outcome according to laboratory and clinical features. Med J Aust. 1996; 165(7): 360-7.
10. Conde-Agudelo A, Belizan JM. Risk factors for pre-eclampsia in a large cohort of Latin America and Caribbean women. BJOG 2000; 107 (1): 75-83.
11. Milne F, Redman C, Walker J, Baker P, Badley J, Cooper C. The pre-eclampsia community guideline (PRECOG): how to screen for and detect onset of Preeclampsia in the community. BMJ 2005; 330:576-580.
12. Nabila N, Sonia S, Nasreen N & Hassan H. Perinatal outcome in high risk pregnancies. JCPSP 2009;19(7):432-5.
13. Lee W, O'Connell CM, Baskett TF. Maternal and perinatal outcomes ofeclampsia: Nova Scotia, 1981-2000.J ObsetGynaecol Can.2004;26(2):119-23.
14. Ros HS, Cnattingius S, Lipworth L. Comparison of risks Factors for Preeclampsia and gestational hypertension in a population based cohort study Am. J. Epidemiol. 1988; 147 (11): 1062-70.
15. Mc Gravy S, Zimmer S,Willett W &Rosner B, Maternal prenataldietary potassium, calcium, magnesium & infant blood pressure.hypertension 1991; 17:218-2.
16. Anath CV, Pidicayil A, Savitz DA. Effect of hypertensive disease in pregnancy on birth weight, gestational duration and small for gestational age birth. Epidemiology 1995; 6(4): 391-5.
17. Xiong X, Mayes D, Demianczuk N, Olson DM, Davidge ST, Newburn-Cook C, et al. Impact of pregnancy-induced hypertension on fetal growth. Am. J. Obstet Gynecol. 1999; 180(1 pt1): 207-13.
18. Helewa ME, Burrows RF, Smith J, Williams, Brain P, Rabkin SW. and classification of hypertensive disorders in Definitions, evaluation pregnancy: Report of the Canadian Hypertension Society Consensus Conference: Can Med Assoc. J. 1997;157 (6): 715-725.
19. Central Bureau of Statistics National Planning Commission. Republic of Namibia 2001 Population & Housing census. National report Basic Analysis with Highlights 2003;11.
20. Sibai BM. Hypertension. In Gabbe SG, Niebyl JR, Galan H, et al (eds). Obstetrics: Normal & Problem Pregnancies, 6th ed. New York: Elseiver, 2012; 779-822.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

