Comparative Study Between Normal Pregnancy Outcome with Pregnancy with Diabetes Mellitus in Rangpur Medical College & Hospital, Rangpur, Bangladesh
Abstract
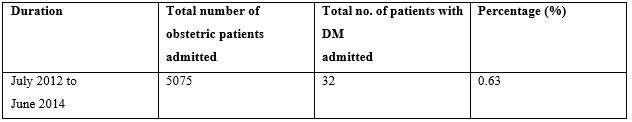
Background: Diabetes mellitus is one of the common medical diseases with pregnancy. Increasing maternal age, overweight, life style change and family history of diabetes are all risk factor for diabetes mellitus. Objectives: To evaluate the foeto-maternal outcome in pregnancy and to compare with the patients having no DM/GDM and any medical disease. Materials and Methods: This is a cross sectional descriptive study which includes both the booked case having pregestational diabetes or newly diagnosed GDM cases admitted directly through the emergency or OPD with or without labour pain. Study period: From February 2015 to August 2015. Results: During the study period total 5075 obstetrics patients were admitted out of them 32(0.63%) were diabetes mellitus with pregnancy. Both age & parity matched study were done between diabetic & control group. Among them 12 (40%) had pregestational diabetes mellitus and 18(53.33%) above the age of 30 years, majority were multipara 15(50%) patients were with the gestatinal age of 38-40 weeks. Majority patients of diabetic group 18(60%) belongs to average socioeconomic status where as in control group 7(23.33%). 11(36.67%) patients diabetic group were secondarily educated in comparison to 06(20%) in control group those are statistically highly significant (p=0.008). Regarding BMI 40% were overweight in diabetic group compare to 16.67% control group that is statistically significant as a whole (p=0.007). There was no significant difference in the rates of foetal birth asphyxia but macrosomic baby in diabetic group in 7.4% caessarean section were 27(90%) in diabetic group compare to 09(30%) in control group that is statistically highly significant (p=0.000). Successful vaginal delivery had done in 10% patients in diabetic group under supervision. Conclusion: In our country DM is not uncommon and it is often associated with higher incidence of maternal and perinatal mortality due to lack of proper antenatat, intranatat and emergency obstetric care.
Downloads
References
2. Jovanovic L, Pettitt DJ: Gestational diabetes mellitus. JAMA 2001, 286:2516 2518.
3. Metzger BE, Coustan DR, eds. Proceedings of the Fourth International Workshop Conference on Gestational Diabetes Mellitus. Diabetes Care 1998 21(Suppl 2):B1-B167.
4. Berkowitz K, Peters R, Kjos SL, Goico J, Marroquin A, Dunn ME, et al. Effect of troglitazone on insulin sensitivity and pancreatic beta-cell function in women at high risk for NIDDM. Diabetes. 1996; 45:1572-9.
5. Sermer M, Nayor C, Kenshole A, et al. The Toronto Tri-Hospital Gestational Diabetes Project: A preliminary review. Diabetes Care. 1998; 21 suppl 2.833- 842.
6. Nirmala Kampan, Hanis Azman, Izzat Hafiz, Hazwani Mohammad, Chuah Su Yee, Nur Azurah AbdGhani, Nor Azlin Mohamed Ismail, Zaleha Mahdy Abdullah. Outcome of pregnancy among malaysian women with diabetes mellitus; Malaysian Journal of Public Health Medicine 2013; Vol. 13 (2):1-10
7. Metal S. 1987. The diabetic pregnancy in: Review of management and results over seven years’ period. Asia Oceania. Am J Obstet&Gynecol: 277-282.
8. Emmanuel odar. Julius Wandabwa, and paulKionda. Maternal and fetal outcome of gestational diabetes mellitus in Mulago Hospital, Uganda.
9. Hayfaa A Wahabi, Samia A Esmaeil, Amel Fayed et al. Pre existing diabetes mellitus & adverse pregnancy outcomes. BMC Sep 10, 2012; 5; 496.
10. Sermer M, Naylor CD, Gare DJ: Impact of increasing carbohydrate metabolism intolerance on maternal fetal outcomes in 3637 women without gestational diabetes: The Toronto tri-hospital gestational diabetes project. Am J ObstetGynecol 1995, 173:146-156.
11. AhiaGarshasbi, SoghratFaghihzadeh, Mohammad Mehdi NaghizadenMandanaGhavam, prevalence and risk factors for gestational diabetes mellitus in Tehran. Journal of family and reproductive health; June 2008; vol. 2(2); 75-79.
12. Farhana J. 1997. Effects of DM on pregnancy outcome. (Dissertation - Obst and Gynaecology) BCPS., 79. Nagy G, 1993, management of gestational diabetes. J Obstet & Gynecol; 115: 147-153.
13. Syed Habeebullah Maternal & fetal outcome in gestational diabetes mellitus treated with diet & metformine. Open conference proceedings journal, 2011: vol. 2: 59-63.
14. Arias F. Diabetes and preagnancy In: Shirish N Daftary, Amarnath G Bhideeds Practical guide to High-Risk Preagnancy and Delivery. 3rd ed New Delhi, India 2008. Elesvier: 440-463.
Copyright (c) 2024 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

