Assessment of serum Lactate Dehydrogenase in preeclamptic pregnant women
Abstract
Background: Evidences prove that endothelial cell and altered endothelial cell function play an important role in the pathogenesis of preeclampsia. Therefore serum lactate dehydrogenase (LDH) is useful biochemical markers reflecting the severity of the occurrence of preeclampsia.
Objective: Determination of serum lactate dehydrogenase (LDH) in severe preeclamptic pregnant women.
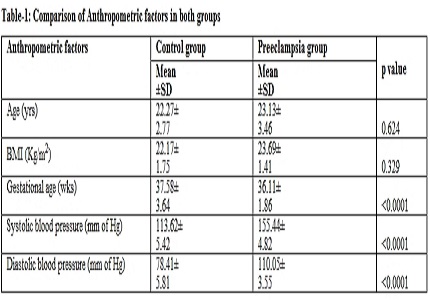
Methods: This is the case-control hospital based study carried in the Al Azhar Medical College and Super speciality Hospital, Thodupuzha. Normal pregnant women (n=55) and women with severe preeclampsia (n=63) were included in the study. Both the groups were in their third trimester and of same age and same gestational age. Serum LDH levels were measured by continuous spectrophotometric pyruvate method for both groups.
Results: Higher values of serum lactate dehydrogenase (LDH) were found in severe preeclamptic women compared with normal pregnant women in third trimester.
Conclusion: Elevated levels of serum LDH indicates the tissue damage and might be the cause of the occurrence of preeclampsia.
Downloads
References
2. WHO, 2004. Bethesda, MD. Global Burden of Disease for the Year 2001 by World Bank Region, for Use in Disease Control Priorities in Developing Countries, National Institutes of Health: WHO. Make every mother and child count. World Health Report, 2005, Geneva: World Health Organization, 2005. 2nd ed. [PubMed]
3. Stekkinger E, Zandstra M, Peeters LL, Spaandernen ME. Early-onset preeclampsia and the prevalence of postpartum metabolic syndrome. Obstet Gynecol. 2009 Nov;114(5):1076-84. doi: 10.1097/AOG.0b013e3181b7b242. [PubMed]
4. Kay HH, Zhu S, Tsoi S. Hypoxia and lactate production in trophoblast cells. Placenta. 2007 Aug-Sep;28(8-9):854-60. Epub 2007 Feb 2. [PubMed]
5. Lopez-Jaramillo P, Casas JP, Serrano N.Preeclampsia: from epidemiology observation to molecular mechanisms. Braz J Med Biol Res. 2001 Oct;34(10):1227-35. [PubMed]
6. Jan AK, Jamil M. Management of preeclampsia and Eclampsia. JPMI 2000;14(1):67-71. [PubMed]
7. Pasaoglu H, Bulduk G, Ogus E, Pasaoglu A et al. Nitric oxide, lipid peroxide and uric acid levels in preeclampsia and eclampsia. Tohoku J Exp Med. 2004 Feb;202(2):87-92. [PubMed]
8. Norwitz ER, Hsu CD, Repke JT. Acute complications of preeclampsia. Clin Obstet Gynecol. 2002 Jun;45(2):308-29. [PubMed]
9. Page NM. The endocrinology of preeclamspia. Clin Endocrinol (Oxf). 2002 Oct;57(4):413-23. [PubMed]
10. Qublan HS, Ammarin V, Bataineh O, Al Shraideh Z,Tahat Y, Awamleh I, et al. Lactic dehydogenase as a biochemical marker of adverse pregnancy outcome in severe preeclampsia. Med Sci Monit. 2005 Aug;11(8):CR393-7. Epub 2005 Jul 25. [PubMed]
11. Krefetz RG: Enzymes. Clinical Chemistry,4th ed. Lippincott Williams and Wikins; Philadelphia 2000;196-98. [PubMed]
12. Malarewicz A, Gruszka O, Szymkiewicz J, Rogala J. The usefulness of routine laboratory tests in the evaluation of sudden threat of pregnant woman and fetus in preeclampsia. Ginekol Pol 2006; 77(4):276-84. [PubMed]
13. Jaiswar SP, Gupta Amrit, Sachan Rekha, Natu SN, Shaili Mohan. Lactic Dehydrogenase: A biochemical marker for preeclampsia-eclampsia. JOGI 2011; 61(6): 645-648. [PubMed]
Copyright (c) 2016 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

