The effect of prophylactic use of intravenous tranexamic acid in abdominal hysterectomy
Abstract
Introduction: Hysterectomy is one of the frequently performed major gynecological surgical procedures for various uterine pathologies. The objective of this study is to assess the effect of intravenous tranexamic acid in reducing intraoperative and postoperative blood loss in women undergoing abdominal hysterectomy.
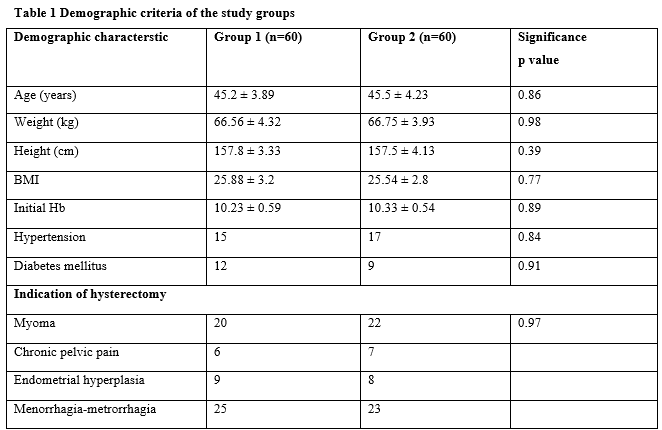
Materials and Methods: The study was a randomized double-blind study, involving a total of 120 women undergoing abdominal hysterectomy for benign etiology were randomly assigned to two groups: Group 1 (non TA): (n=60) women receiving normal saline and Group 2 (TA): (n=60) women receiving prophylactic Tranexamic Acid in 100 ml saline IV just before skin incision. The primary outcome was intraoperative, postoperative, and all blood loss estimation.
Results: Group 2 (TA) showed a great reduction in intraoperative and postoperative blood loss (blood in the intra-abdominal drain) compared with Group 1 (non TA), (P = 0.0001, 0.0001), so the overall estimated blood loss in groups 2 showed significant reduction compared with Group 1 (P = 0.0001).
Conclusion: Intravenous tranexamic acid is a safe and reliable method to help decrease blood loss during and after abdominal hysterectomy.
Downloads
References
Murphy WG, Davies MJ, Eduardo A. The haemostatic response to surgery and trauma. Br J Anaesth. 1993; 70(2):205-13. doi: 10.1093/bja/70.2.205.
Levy JH, Dutton RP, Hemphill JC, Shander A, Cooper D, Paidas MJ. Hemostasis Summit Participants: Multidisciplinary approach to the challenge of hemostasis. Anesth Analg. 2010; 110(2):354-64. doi: 10.1213/ANE.0b013e3181c84ba5.
Wellington K, Wagstaff AJ. Tranexamic acid: Review of its use in management of menorrhagia. Drugs. 2003; 63(13):1417-33. doi: 10.2165/00003495-200363130-00008.
Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010; 376(9734):23-32. doi: 10.1016/S0140-6736(10)60835-5.
Roberts I, Fawole B, Chaudhri R, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial WOMAN Trial Collaborators. The Lancet. 2017;389(10084):2105–16. doi: 10.1016/S0140-6736(17)30638-4.
Topsoee MF, Bergholt T, Ravn P, et al. Anti-hemorrhagic effect of prophylactic tranexamic acid in benign hysterectomy—a double-blinded randomized placebo-controlled trial. Am J Obstet Gynecol. 2016; 215(1):72.e1-8. doi: 10.1016/j.ajog.2016.01.184.
Essola L, Koue´gnigan Re´rambiah L, Obame R, et al. Can venous iron and tranexamic acid reduce the transfusion need? Report on a non-randomized, case control study. Transfus Clin Biol. 2017;24(2):52–5. doi: 10.1016/j.tracli.2017.01.002.
Shady NW, Sallam HF, Fahmy H. Reducing blood loss during open myomectomy with intravenous versus topical tranexamic acid: A double-blinded randomized placebo-controlled trial. Middle East FertilSoc J. 2018;7(9):3538-3545. doi: 10.1007/s13224-018-1149-x.
Henry DA, Carless PA, Moxey AJ, et al. Antifibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2011: (1):CD001886. doi: 10.1002/14651858.CD001886.pub3.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

