Management of Postpartum Haemorrhage: A study on Transfusion of Blood and its components
Abstract
Introduction: Blood Transfusion is identified as one of the essential components of comprehensive emergency obstetric care which has drastically reduced maternal mortality.
Material and Methods: This is a prospective study conducted at NC Medical College and Hospital, in the Department of OBGY. (Tertiary care center) from January 2019 – September 2020. All patients requiring intrapartum transfusion of blood or blood products are enrolled in the study. No exclusion criteria.
Results: In the present study, various age groups of patients were enrolled. Maximum transfusion (77.8%) rates are seen in the age group of 21-30 years and the minimum no. of patients were ranges from 31-40 years (8.4%).
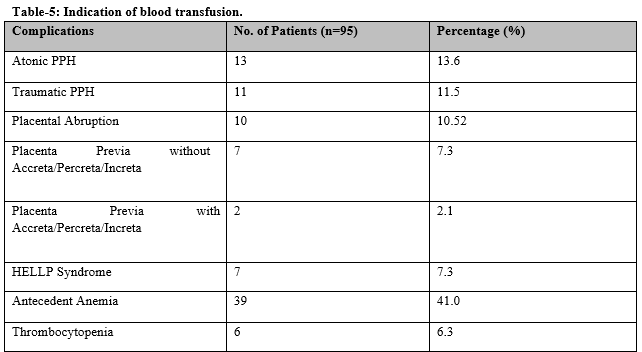
Conclusion: Postpartum hemorrhage, placental causes, and anemia are the commonest causes of the need for transfusion in obstetric practice.
Downloads
References
Karpati PC, Rossignol M, Pirot M, Cholley B, Vicaut E, Henry P, et al. High incidence of myocardial ischemia during postpartum hemorrhage. Anesthesiol. 2004;100(1):30-36. doi: 10.1097/00000542-200401000-00009.
Kalaivani K. Prevalence & consequences of anaemia in pregnancy. Indian J Med Res. 2009;130(5):627-633. doi: 10.18203/2320-1770.ijrcog20180155.
Bomken C, Mathai S, Biss T, Loughney A, Hanley J. Recombinant activated factor VII (rFVIIa) in the management of major obstetric haemorrhage: a case series and a proposed guideline for use. Obstet Gynecol Int. 2009;364843. 1-8. doi: 10.1155/2009/364843.
Parker J, Thompson J, Stanworth S. A retrospective oneyear single-centre survey of obstetric red cell transfusions. Int J Obstet Anesth. 2009;18(4):309-313. doi: 10.1016/j.ijoa.2009.05.008.
Rainaldi MP, Tazzari PL, Scagliarini G, Borghi B, Conte R. Blood salvage during caesarean section. Br J Anaesth. 1998;80 (2):195-198. doi: 10.1093/bja/80.2.195
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: Postpartum hemorrhage. Obstet Gynecol. 2006;108(4):1039-1047. doi: 10.1097/00006250-200610000-00046.
Alfirevic Z, Elbourne D, Pavord S, Bolte A, Van Geijn H, Mercier F, et al. Use of recombinant activated factor VII in primary postpartum hemorrhage: the Northern European registry 2000-2004. Obstet Gynecol. 2007;110(6):1270-1278. doi: 10.1097/01.AOG.0000288515.48066.99.
McGehee RP, Dodson MK, Moore JL, Morrison FS et al. Effect of blood transfusion in patients with gynaecologic malignancy. Int J Obstet Gynecol. 1994;46(1):45-52. doi: 10.1016/0020-7292(94)90308-5.
Santoso JT, Saunders BA, Grosshart K. Massive blood loss and transfusion in obstetrics and gynecology. Obstet Gynecol Surv. 2005;60(1):827-37. doi: 10.1097/01.ogx.0000189154.98227.4b
Voak D. Guidelines for administration of blood products: transfusion of infants and neonates. British Committee for Standards in Haematology Task Force. Transfusion Med. 1994;4(1):63-69. doi: 10.1111/j.1365-3148.1994.tb00245.x.
Dickason LA, Dinsmoor MJ. Red blood cell transfusion and caesarean section. Am Jobstet Gynecol. 1992;167(2):327-330. doi: 10.1016/s0002-9378(11)91409-4.
Saxena S, Rabinowitz AP, Johnson C, Shulman IA. Iron-deficiency anaemia: a medically treatable chronic anaemia as a model of transfusion overuse. Am J Med. 1993;94(2):120-124. doi: 10.1016/0002-9343(93)90172-l.
Borghi B, van Oven H. Reducing the risk of allogeneic blood transfusion. CMAJ. 2002;166(3):332-334.
Adias TC, Jeremiah Z, Uko E, Osaro E. Autologous blood transfusion – A review. S Afr J Surg. 2006;44(3):114-116. doi: 10.1016/s0002-9378(11)91633-0.
Droste S, Sorensen T, Price T, Sayers M, Benedetti T, Easterling T, et al. Maternal and fetal hemodynamic effects of autologous blood donation during pregnancy. Am J Obstet Gynecol. 1992;167(1):89-93. doi: 10.1016/s0002-9378(11)91633-0.
Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. First of two parts – Blood transfusion. N Engl J Med. 1999;340(6):438-447. doi: 10.1056/NEJM199902113400606.
Yamada T, Mori H, Ueki M. Autologous blood transfusion in patients with placenta previa. Acta Obstet Gynecol Scand. 2005;84(3):255-259. doi: 10.1111/j.0001-6349.2005.00698.x.
Fuller AJ, Bucklin B. Blood component therapy in obstetrics. Obstet Gynecol Clin North Am 2007;34(3):443-458. doi:10.1016/j.ogc.2007.06.003.
Alfirevic Z, Elbourne D, Pavord S, Bolte A, Van Geijn H, Mercier F, et al. Use of recombinant activated factor VII in primary postpartum hemorrhage: the Northern European registry 2000-2004. Obstet Gyneco.l 2007;110(6):1270-1278. doi: 10.1097/01.AOG.0000288515.48066.99.
Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H, et al.; PPH Study Group. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007;5(2):266–273. doi: 10.1111/j.1538-7836.2007.02297.x.
Koshy M, Burd L, Wallace D, Moawad A, Baron J. Prophylactic red cell transfusions in pregnant patients with sickle cell disease. A randomised cooperative study. N Engl J Med. 1988;319(22):1447-1452. doi: 10.1056/nejm198812013192204.
Carless PA, Henry DA, Moxey AJ, O’connell DL, Brown T, Fergusson DA. Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2006;18(4):CD001888. doi: 10.1002/14651858.CD001888.pub2.
Clark V. Facilities for blood salvage (cell saver technique) must be available in every obstetric theatre. Int J Obstet Anesth. 2005;14(1):48-50. doi: 10.1016/j.ijoa.2004.09.001.
Rebarber A, Lonser R, Jackson S, Copel JA, Sipes S. The safety of intraoperative autologous blood collection and autotransfusion during cesarean section. Am J Obstet Gynecol. 1998;179(3 pt 1):715-720. doi: 10.1016/s0002-9378(98)70070-5.
Murphy MF, Wallington TB, Kelsey P, Boulton F, Bruce M, Cohen H, et al.; British Committee for Standards in Haematology, Blood Transfusion Task Force. Guidelines for the clinical use of red cell transfusions. Br J Haematol. 2001;113(1):24-31. doi: 10.1046/j.1365-2141.2001.02701.x.
Iwamoto M, Jernigan DB, Guasch A, Trepka MJ, Blackmore CG, Hellinger WC, et al. Transmission of West Nile virus from an organ donor to four transplant recipients. New Engl J Med. 2003;348(22):2196-203. doi: 10.1056/NEJMoa022987.
Bomken C, Mathai S, Biss T, Loughney A, Hanley J. Recombinant activated factor VII (rFVIIa) in the management of major obstetric haemorrhage: a case series and a proposed guideline for use. Obstet Gynecol Int. 2009;2009:364843. doi: 10.1155/2009/364843.
Prendiville WJ, Elbourne D, McDonald S. Active versus expectant management in the third stage of labour. Cochrane Database Syst Rev. 2000;(2):CD000007. doi: 10.1002/14651858.CD000007.
Franchini M, Franchi M, Bergamini V, Montagnana M, Salvagno GL, Targher G, et al. The use of recombinant activated FVII in postpartum hemorrhage. Clin Obstet Gynecol. 2007;114(1):8-15. doi: 10.1111/j.1471-0528.2006.01156.x.
Copyright (c) 2021 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

