A Comparison of efficacy of I/V Iron V/S Oral Iron for management of iron deficiency anemia in pregnant women in a tertiary care center
Abstract
Introduction: WHO defines anemia in pregnant women as hemoglobin level <11gm/dL and a hematocrit of <0.33. The number of patients with iron deficiency anemia is>2 billion which accounts for 30% of the world’s population. The incidence of iron deficiency anemia in India is around 50%.
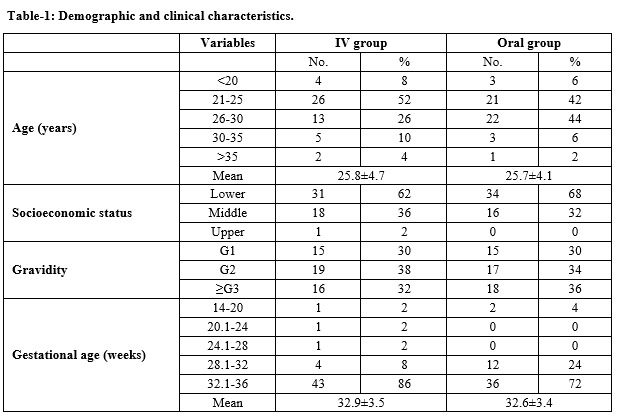
Material and Methods: A study was performed in the Department of Obstetrics and Gynecology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India on 100 antenatal patients with nutritional anemia gestational age of 14-36 weeks. Group A was treated with intravenous iron sucrose and group B was treated with oral iron sulfate. Pretreatment hemoglobin, S. ferritin levels, and General Blood Picture were recorded. During the course of treatment, any adverse reactions with either formulation, if occurred were recorded. Patients were followed up after 4 weeks with repeat hemoglobin and S. ferritin level.
Results: The mean improvement of hemoglobin among I/V and Oral iron following treatment was 1.68±0.33 gm/dl and 0.96± 0.31 gm/dl respectively which was statistically significant. The improvement in iron stores was also observed more in the I/V group with a rise of S. ferritin of 27.21±9.5 ng/ml against a rise of 3.72± 0.7 ng/ml in the oral group. This was statistically significant with a P-value of 0.000 in the I/V group. No major adverse reactions were seen in both groups.
Conclusion: Intravenous iron sucrose is safe and more effective than oral iron therapy in the treatment of iron deficiency anemia and to restore iron stores in pregnant women.
Downloads
References
De benoist B.(eds). Worldwide Prevalence of anemia 1993-2005. WHO Global Database on Anemia Geneva, 2008. Available at https://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/9789241596657/en/.
Bhat R. Maternal mortality in India-FOGSI-WHO study. J Obstet Gynaecol India .1997;47(3):207-214.
Kumar A, Jain S, Singh NP, Singh T. Oral versus high dose parentral iron supplementation in pregnancy. Int J Gynecol Obstet. 2005;89(1):7-13. doi: 10.1016/j.ijgo.2005.01.016.
Malagi U, Reddy M, Naik R. Evaluation of national nutritional control programme in Dharward (Karnataka). J Hum Ecol. 2006;20(4):279-281. doi: 10.1080/09709274.2006.11905939.
Khurana A. Ultrasound in obstetric practice. Ian Donald’s Practical Obstetrics Problems, 9/e. 2020 May 1:61.
Pathak P, Kapil U, Kapoor S.K, Saxena R. Indian J Pediatr. 2004;71(11):1007-1014. doi: 10.1007/BF02828117.
Zama I, Argungu IB, Yakubu A, Taylor JR, Erhabor O, Suzette U. Socio-demographic and obstetric factors associated with anemia among pregnant women in Sokoto, North Western Nigeria. Am Assoc Sci Technol. 2014;1(5):119-126.
Ahmed N, Kalakoti P, Bano R, Syed MMA. The prevalence of anaemia and associated factors in pregnant women in a rural Indian community. Aust Med J. 2010;5(3):276-280. doi: 10.4066/AMJ.2010.286.
Aggarwal RS, Mishra VV, Panchal NA, Patel NH, Deshchougule VV, Jasani AF. Evaluation of iron sucrose and oral iron in the management of Iron Deficiency Aaemia in pregnancy. Nat J Comm Med. 2012;93(1):415-416.
Rudra S, Chandna A, Nath J. Comparison of intravenous iron sucrose with oral iron in pregnant women with iron deficiency anemia. Int J Reprod Contracept Obstet Gynecol. 2016;5(3):747-751. doi: 10.18203/2320-1770.ijrcog20160577.
Tandon A, Gupta V, Chaudhary P, Kumari N. Comparison between intravenous iron sucrose versus oral iron iron therapy in pregnant women with nutritional anemia: a prospective study. Int J Reprod Contracept Obstet Gynecol. 2016;5(7):2278-2281. doi: 10.18203/2320-1770.ijrcog20162110.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

