Association between body mass index and dysmenorrhea among medical students: A cross-sectional study
Abstract
Background and Aim: The etiology of menstrual disorders such as dysmenorrhea, premenstrual symptoms, menorrhagia, polymenorrhea, abnormal vaginal bleeding, amenorrhea, oligomenorrhea, and irregular menstruation among the can be due to various psychological as well as organic causes. This study was conducted to assess the menstrual pattern in young adult females.
Material and Methods: A cross-sectional study was conducted among female MBBS students and interns of Gujarat Adani Institute of Medical Science Bhuj, Kutch, Gujarat, India. Data was collected in a semi-structured questionnaire that was administered to all undergraduate female medical students in the age group of 18-25years. The questionnaire consisted of details regarding the menstrual history- the duration and amount of flow of the recent three menstrual cycles, associated symptoms like dysmenorrhoea, leg cramps, and any other bodily changes like weight gain, hair growth, etc was taken. These students' anthropometric measurements such as height, weight BMI, any signs of hirsutism, or androgenic were recorded.
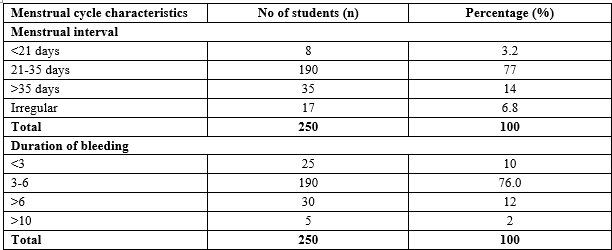
Results: 2.9% of the students had polymenorrhoea. Oligomenorrhoea was found in 14% of participants. The length of the menstrual interval was normal (i.e. 21-35 days) in 76% of the students whereas 6.8% of students had an irregular menstrual cycle. It was found that a high percentage (66.6%) of students who were overweight/obese were reportedly suffering from dysmenorrhea. Whereas lesser percentage underweight (44.7%) and normal weight (55.5%) students were reportedly suffering from dysmenorrhea.
Conclusion: Early diagnosis and management of dysmenorrhea should be done and appropriate necessary lifestyle modification should be encouraged among young females to reduce the incidence of PCOD and metabolic syndrome later in life.
Downloads
References
Beek, Jonathan S. Puberty and dysmenorrhea treatment: In Novak’s Gynecology. London: Williams and Wilkins publication Inc. 14th Ed, 2006: p 1696.
Omidvar S, Begum K. Menstrual pattern among unmarried women from south India. J Nat Sci Biol Med. 2011;2(2):174-179. Available from: http://www.jnsbm.org/text.asp?2011/2/2/174/92329.
Reed BG, Carr BR. The normal menstrual cycle and the control of ovulation. InEndo text. 2018.
Godbole G, Phadake A, Joshi AR. Pattern of menstrual cycle in young adults. Indian J Basic Appl Med Res. 2013;2(8):1017-1021.
Sood M, Devi A, Daher A, Razali S, Nawawi H, Hashim S, et al. Poor Correlation of Stress Levels and Menstrual Patterns among Medical Students. J ASIAN Behav Stud. 2017;2(5):73-78. doi: http://dx.doi.org/10.21834/jabs.v2i5.221.
Allen SS, Allen AM, Tosun N, Lunos S, Al'absi M, Hatsukami D. Smoking- and menstrual-related symptomatology during short-term smoking abstinence by menstrual phase and depressive symptoms. Addict Behav. 2014;39(5):901-906. doi: https://doi.org/10.1016/j.addbeh.2014.01.029.
Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. 2014;36 (1):104-113. doi: https://doi.org/10.1093/epirev/mxt009.
Barnard K, Frayne SM, Skinner KM, Sullivan LM. Health status among women with menstrual symptoms. J Women's Health. 2003;12(9):911-919. doi: https://doi.org/10.1089/154099903770948140.
Antherjanam SD, Karunakaran U, Jayasree AK., Antony R, Anitha SS, Harsha CH. Prevalence and pattern of menstrual disorders among school going adolescents in northern district of Kerala. Public Health Rev. 2016;3(3):109-118. Available from: https://publichealth.medresearch.in/index.php/ijphr/article/view/40.
Lentz G, Lobo R, Gershenson D, Katz V. Comprehensive Gynecology. Philadelphia: Mosby Elsevier. 6th ed; 2013.
Khodakarami B, Masoomi SZ, Faradmal J, Nazari M, Saadati M, Sharifi F, et al. The severity of dysmenorrhea and its relationship with body mass index among female adolescents in Hamadan, Iran. J Midwifery Reprod Health. 2015;3(4):444-450. doi: https://dx.doi.org/10.22038/jmrh.2015.4618.
Barnard K, Frayne SM, Skinner KM, Sullivan LM. Health status among women with menstrual symptoms. J Womens Health (Larchmt). 2003;12(9):911-919. doi: https://doi.org/10.1089/154099903770948140.
Bettendorf B, Shay S, Tu F. Dysmenorrhea: Contemporary perspectives. Obstet Gynecol Surv. 2008;63(9):597-603. doi: https://doi.org/10.1097/ogx.0b013e31817f15ff.
Berek JS. Berek and Novak’s Gynecology. Philadelphia: Lippincott, Williams & Wilkins. 15th ed, 2011.
Gibbs RS, Karlan BY, Haney AF, Nygaard IE. Danforth’s Obstetrics and Gynecology. Philadelphia: Lippincott, Williams & Wilkins. 10th ed, 2008.
Schuiling KD, Likis FE. Women’s Gynecologic Health. Massachusetts: Jones & Bartlett Learning. 2nd ed, 2011.
Salmalian H, Saghebi R, Moghadamnia AA, Bijani A, Faramarzi M, NasiriAmiri F, et al. Comparative effect of thymus vulgaris and ibuprofen on primary dysmenorrhea: A triple-blind clinical study. Caspian J Intern Med. 2014;5(2):82-88.
Eittah HF. Effect of breakfast skipping on young females’ menstruation. Health Sci J. 2014;8(4):469-484.
Wallace S, Keightley A, Gie C. Dysmenorrhoea. Obstet Gynaecol. 2010;12:149-154.
Akerlund M, Strömberg P, Forsling ML. Primary dysmenorrhoea and vasopressin. Br J Obstet Gynaecol. 1979;86(6):484-487. doi: https://doi.org/10.1111/j.1471-0528.1979.tb10794.x.
Hirata M, Kumabe K, Inove Y. Study of relation between frequency of menstrual pain and body weight in female adolescents. Nippon Koshu Eisei Zasshi. 2002;49(6):516-524.
Tangchai K, Titapant V, Boriboonhirunsarn D. Dysmenorrhea in Thai adolescents: Prevalence, impact and knowledge of treatment. J Med Assoc Thai. 2004;87(3):S69-S73.
Dambhare DG, Wagh SV, Dudhe JY. Age at menarche and menstrual cycle pattern among school adolescent girls in Central India. Glob J Health Sci. 2012;4(1):105. doi: https://doi.org/10.5539/gjhs.v4n1p105.
Agarwal A, Venkat A. No Title. J Ped Adolesc Gyn. 2009;22(6):365-371. doi: https://doi.org/10.1016/j.jpag.2009.02.005.
Nisar N, Zehra N, Haider G, Munir A, Sohoo NA. Frequency, Intensity and Impact of Premenstrual Syndrome in Medical Students. J Coll Physicians Surg Pakistan. 2008;18(8):481-484.
Bettendorf B, Shay S, Tu F. Dysmenorrhea: Contemporary perspectives. Obstet Gynecol Surv. 2008;63(9):597-603. doi: https://doi.org/10.1097/ogx.0b013e31817f15ff.
Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Prevalence of polycystic ovarian syndrome in Indian adolescents. J Pediatr Adolesc Gynecol. 2011;24(4):223-227. doi: https://doi.org/10.1016/j.jpag.2011.03.002.
Gill H, Tiwari P, Dabadghao P. Prevalence of polycystic ovary syndrome in young women from North India: A Community-based study. Indian J Endocrinol Metab. 2012;16(2):389-392. doi: https://doi.org/10.4103/2230-8210.104104.
Chakrabarti M, Rahaman A, Basu SP. Ultrasonographic Prevalence of Polycystic Ovarian Disease – A Cross-Sectional Study in a Rural Medical College of West Bengal. IOSR J Dent Med Sci. 2016;15(1):115-120. doi: https://doi.org/10.9790/0853-15110115120.
Yildiz BO, Knochenhauer ES, Azziz R. Impact of Obesity on the Risk for Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2008;93(1):162-168. doi: https://doi.org/10.1210/jc.2007-1834.
Choudhary A, Jain S, Chaudhari P. Prevalence and symptomatology of polycystic ovarian syndrome in Indian women : is there a rising incidence ? Int J Reprod Contracept Obs Gynecol. 2017;6(11):4971-4975. doi: http://dx.doi.org/10.18203/2320-1770.ijrcog20175010.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

