Effect of daily versus intermittent iron therapy in pregnant women: hematological and pregnancy outcome
Abstract
Background: The purpose of this study was to compare daily iron supplementation and intermittent iron supplementation in preventing anemia in healthy pregnant women.
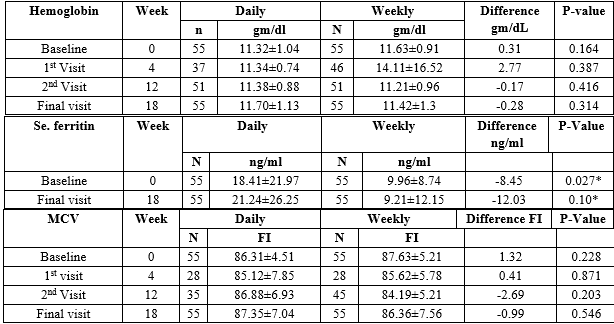
Material and Method: Prospective Randomized Clinical Trial. From May 2004 – December 2006, 141 healthy pregnant women without anemia, between 14 - 20 weeks of pregnancy were randomly allocated into two equal groups. Completed data were obtained in 110 patients, 55 in each group. The first group (n = 55) received a 100 mg-ferrous sulfate tablet daily, the second group (n = 55) received a 100 mg-ferrous sulfate tablet two tablets once weekly, respectively till delivery. Serum hemoglobin, ferritin, and iron were measured before and after the supplementation. Paired t and ANOVA tests were used as appropriate.
Results: There were no significant differences between the pre- and post-treatment hemoglobin levels (p= 0.871) and serum ferritin levels (p= 0.741) with iron supplementation in the two groups when the maternal hemoglobin level was >11g/dL before enrolment. However, For those women who had a hemoglobin concentration <11gm/dL at the beginning, the rise in hemoglobin concentration was significantly greater at the end in the daily supplemented group as compared to the weekly group (1.44±1.51 gm/dl vs. 0.12±1.05 gm/dl, p=0.015). Although when the changes in the serum ferritin level which occurred in each group were compared, there was no significant difference (p=0.415) between the two intervention groups.
Conclusions: These results suggest, daily or weekly iron supplementation is equally effective for healthy pregnant women without anemia.
Downloads
References
Vijayaraghavan K, Brahmam GN, Nair KM, Akbar D, Rao NP. Evaluation of national nutritional anemia prophylaxis programme. Indian J Pediatr. 1990;57(2):183-190. doi: https://doi.org/10.1007/bf02722084.
Solomons NW, Pineda O, Viteri FE, Sandstead HH. Studies on the bioavailability of zinc in humans: mechanism of the intestinal interaction of non-heme Fe and Zinc. J Nutr. 1983;113(2):927-935. doi: https://doi.org/10.1093/jn/113.2.337.
O’”Neil-Cutting MA, Crosby WH. Blocking of iron absorption by a preliminary oral dose of iron. Arch Intern Med. 1987;147(3):489-491.
Viteri FE. Weekly compared with daily iron supplementation. Am J Clin Nutr. 1996;63(4):610-611. doi: https://doi.org/10.1093/ajcn/63.4.610.
Viteri FE. A new concept in the control of iron deficiency: community based preventive supplementation of at risk groups by the weekly intermittent iron supplements. Biomed Environ Sci. 1998:11(1):46-60.
Ridwan E, Schultink W, Dillon D, Gross R. Effects of Weekly iron supplementation on pregnant Indonesian women are similar to those of daily supplementation. Am J Clin Nutr. 1996;63(6):884-890. doi: https://doi.org/10.1093/ajcn/63.6.884.
Liu XN, Zhang JL, Yen HL, Viteri FE. Haemoglobin and serum ferritin levels in pregnant Chinese women in response to weekly iron supplements. [Abstract] In:7th Asian Congress of Nutrition. Beijing, 1995.
Young MW, Lupafya E, Kapendra E, Bobrow E. The effectiveness of weekly iron supplementation in pregnant women of rural northern Malawi. Tropical Doctor 2000;30(2):84-88. doi: https://doi.org/10.1177/004947550003000210.
Rajaratnam J, Abel R, Ganesan C, Jayaseelan SA. Maternal anaemia: A persistent problem in rural Tamil Nadu. Natl Med J Ind. 2000;13(5):242-245.
World Health Organization. The prevalence of anaemia in women: a tabulation of available information. 2nd ed: WHO; Geneva 1992 (WHO/MCH/MSM 92.2). Available at https://apps.who.int/iris/handle/10665/58994.
Svanberg B. Iron absorption in early pregnancy – a study of the absorption of non-haem iron and ferrous iron in early pregnancy. Actabstet Gynecol Scand. 1975;48:69-85. doi: https://doi.org/10.3109/00016347509156331.
Taylor DJ, Ling T. Haematological changes during normal pregnancy: Iron induced macrocytes: Br J Obstet Gynaecol 1976:83(10):760-767. doi: https://doi.org/10.1111/j.1471-0528.1976.tb00740.x.
Taylor DJ, Lind T. Red cell mass during and after normal pregnancy. Br J Obstet Gynaecol. 1979;86(5):364-370. doi: https://doi.org/10.1111/j.1471-0528.1979.tb10611.x.
Stoltzfus RJ, Dreyfuss ML. Guidelines for the use of iron supplements to prevent and treat iron deficiency anemia. Washington, DC: Ilsi Press; 1998. Available at https://motherchildnutrition.org/nutrition-protection-promotion/pdf/mcn-guidelines-for-iron-supplementation.pdf.
Beaton GH, McCabe GP, Micronutrient Initiative. Efficacy of intermittent iron supplementation in the control of iron deficiency anaemia in developing countries: an analysis of experience; final report to the Micronutrient Initiative. Micronutrient Initiative, Ottawa, ON, CA; 1999. Available at https://idl-bnc-idrc.dspacedirect.org/bitstream/handle/10625/29662/117067.pdf?sequence=3.
Agarwal KN, Gomber S, Bisht H, Som M. Anemia prophylaxis in adolescent school girls by weekly or daily iron-folate supplementation. Indian Pediatr. 2003;40(4):296-302.
Mukhopadhyay A, Bhatla N, Kriplani A, Pandey RM, Saxena R. Daily versus intermittent iron supplementation in pregnant women: hematological and pregnancy outcome. J Obstet Gynaecol Res. 2004;30(6):409-417. doi: https://doi.org/10.1111/j.1447-0756.2004.00223.x.
Rajaratnam J, Abel R, Ganesan C, Jayaseelan SA. Maternal anaemia: a persistent problem in rural Tamil Nadu. Nat Med J India. 2000 ;13(5):242-245.
Beard JL. Weekly iron intervention: the case for intermittent iron supplementation. Am J Clin Nutr. 1998;68(2):209-121. doi: https://doi.org/10.1093/ajcn/68.2.209.
Younes M, Eberhrdt I, Lemoine R. Effect of iron overload on spontaneous and xenobiotic induced lipid peroxidation in vivo. J Appl Toxicol. 1989;9(2):103-108. doi: https://doi.org/10.1002/jat.2550090206.
Knutson MD, Walter PB, Ames BN, Viteri FE. Both iron deficiency and daily iron supplements lipid peroxidation in rats. J Nutr. 2000;130(3):621-628. doi: https://doi.org/10.1093/jn/130.3.621.
Viteri FE, Xunian L, Tolomei K, Martin A. True absorption and retention of supplementation iron is more efficient when iron is administered every three days rather than daily to iron- normal and iron deficient rats. J Nutr. 1995;125(1):82-91. doi: https://doi.org/10.1093/jn/125.1.82.
Schultink W, Gross R, Gliwitzki M, Karyadi D, Matulessi P. effect of daily vs twice weekly iron supplementation in Indonesian preschool children with low iron status. Am J Clin Nutr. 1995;61(1):111-115. doi: https://doi.org/10.1093/ajcn/61.1.111.
Beard JL. Effectiveness and strategies of iron supplementation during pregnancy. Am J Clin Nutr. 2000;71(5):1288S-1294S. doi: https://doi.org/10.1093/ajcn/71.5.1288s.
Mumtaz Z, Shahab S, Butt N, Ral MA, DeMuynck A. Daily iron supplementation is more effective than twice weekly iron supplementation in pregnant women in Pakistan in a randomized double-blind clinical trial. J Nutr. 2000;130(11):2697-2702. doi: https://doi.org/10.1093/jn/130.11.2697.
Agarwal A, Rai S, Prasad R. Impact of the Integrated Child Development Services (ICDS) on Maternal Nutrition and Birth Weight in Rural Varanasi KN Agarwal, DK Agarwal. Indian Pediatr. 2000;37(12):1321-1327.
Bhargava M, Iyer PU, Kumar R. Relationship of maternal serum ferritin with foetal serum ferritin, birth weight and gestation. J Trop Pediatr. 1991;37(4):149-152. doi: https://doi.org/10.1093/tropej/37.4.149.
Copyright (c) 2020 Author (s). Published by Siddharth Health Research and Social Welfare Society

This work is licensed under a Creative Commons Attribution 4.0 International License.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative



















 Therapoid
Therapoid

