The Obstetric Risk and Neonatal Consequences of Adolescent Pregnancy
Rahman S1*, Choudhury FH2, Jahan N3, Hasan MM4
DOI:https://doi.org/10.17511/joog.2024.i01.06
1* Silvia Rahman, Assistant Professor, Department of Gynae and Obs, Monno Medical College and Hospital Manikganj, Dhaka, Bangladesh.
2 Farhana Haque Choudhury, Associate Professor, Department of Gynae and Obs, Monno Medical College and Hospital Manikganj, Bangladesh.
3 Nusrat Jahan, Consultant, Department of Gynae and Obs, Feni Medinova Specialised Hospital, Feni, Bangladesh.
4 Md Mehedi Hasan, Assistant Professor, Department of Anesthesia, Monno Medical College and Hospital, Manikganj, Bangladesh.
Introduction: Adolescent pregnancy is a worldwide problem bearing serious social and medical implications relating to maternal and child health. Adolescent pregnancy is a complex and frustrating problem in both developed and developing countries.
Methods: A Cross-sectional observational study was carried out in the Department of Obstetrics and Gynecology; Dhaka Medical College & Hospital, Dhaka, a tertiary-level hospital in Bangladesh from 1st July 2015 to 31st December 2015. 50 patients presented with adolescent pregnancy (Primigravida without medical complications) diagnosed on clinical, biochemical, and investigational backgrounds were enrolled in the study, fulfilling the inclusion and exclusion criteria.
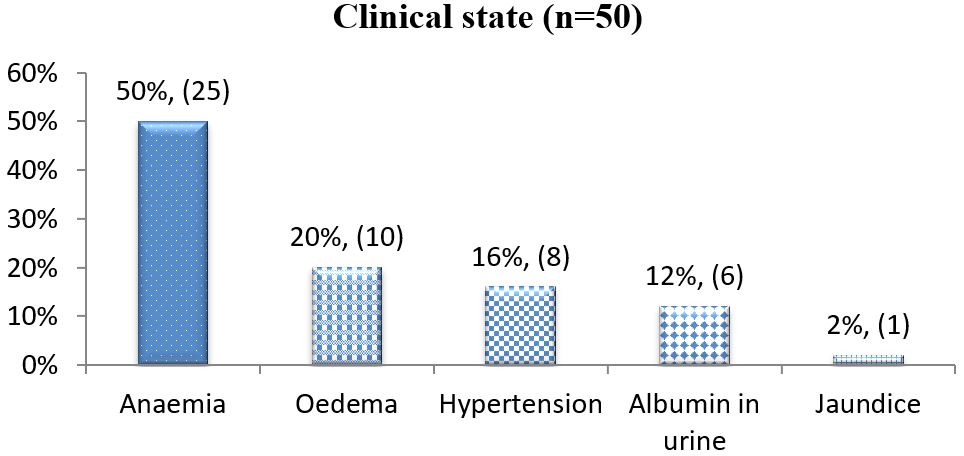
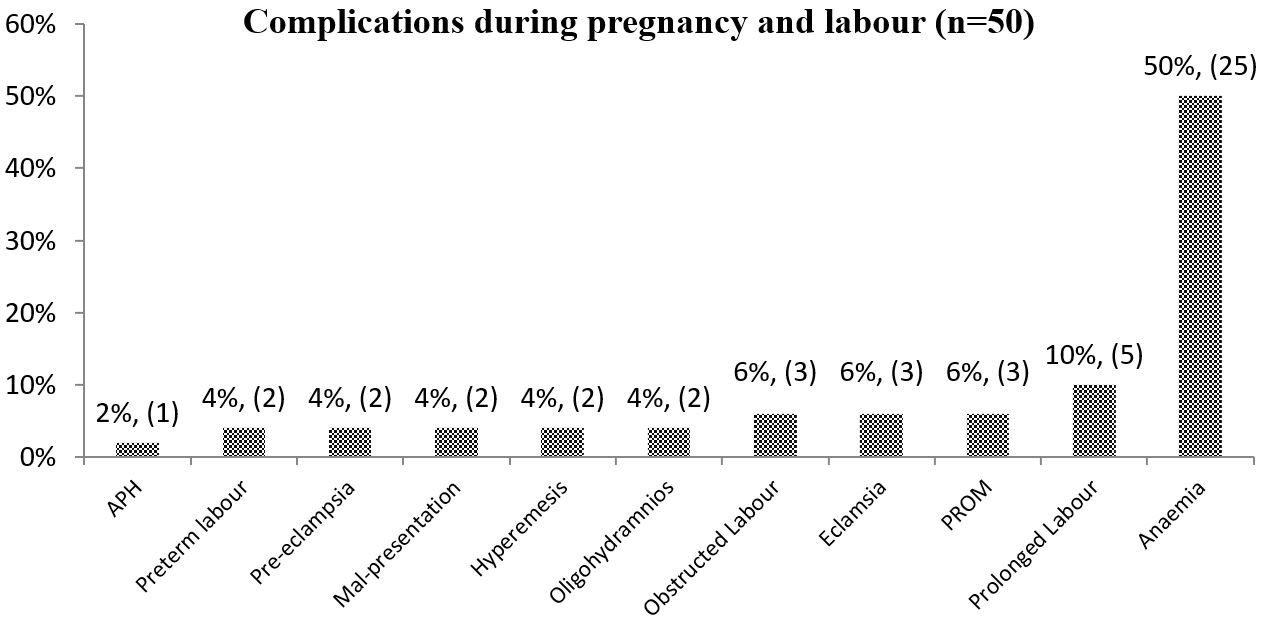
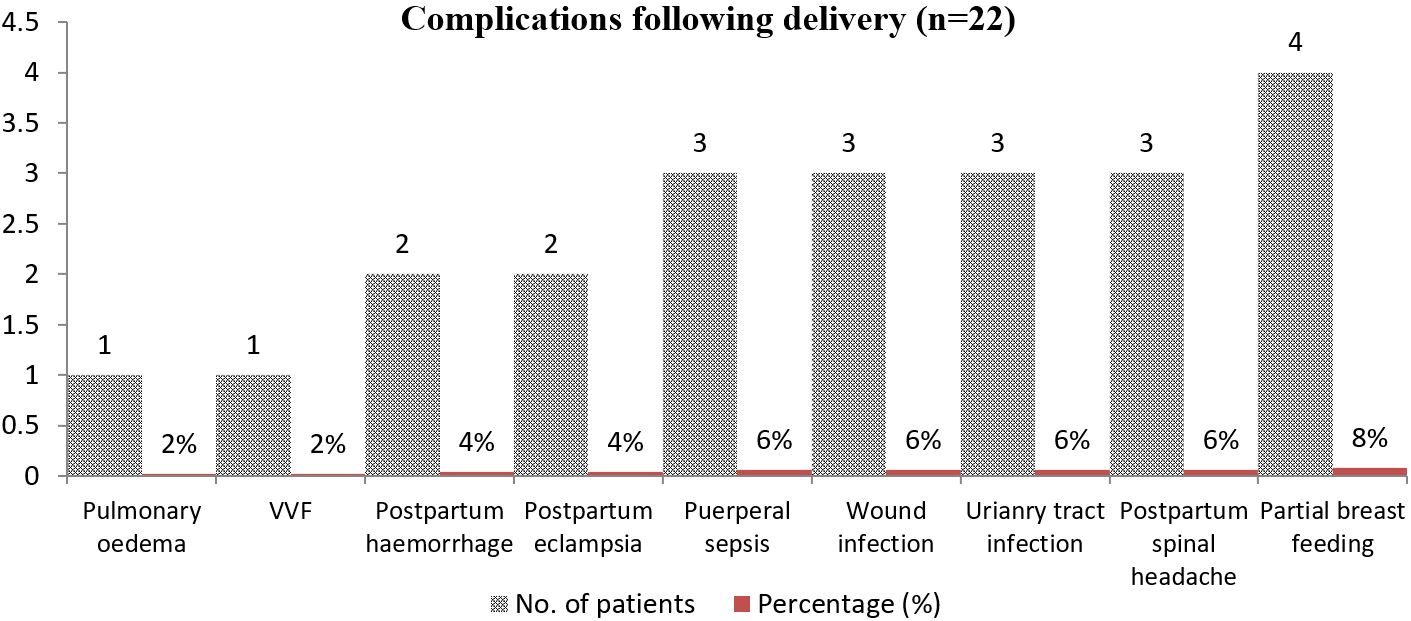
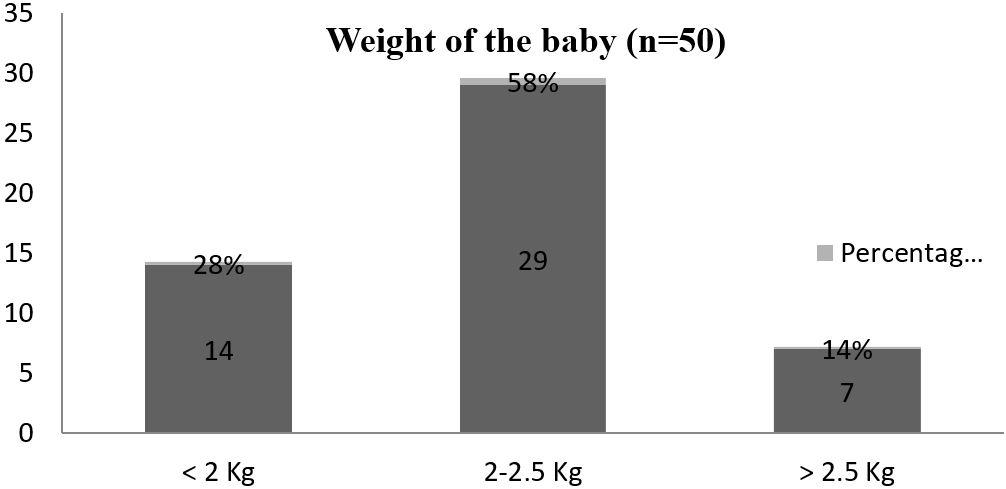
Results: It revealed that the maximum number of teenage patients 44(88%) were between the age group of 17 to 19 years. The present study showed that the majority of teenage mothers were Muslim 43(86%). Most of the teenage mothers were housewives 42(84%), then garments worker 4(8%), then day labourer 2(4%), maid servants 1(2%), student 1(2%). The study also showed that 68% of teenage mothers belong to the monthly income group below TK. 3000; in other words, most of the teenage mothers had come from a low socioeconomic class. Clinical examination findings showed 25(50%) of teenage mothers were anaemic, 10(20%) had oedema, 8(16%) were hypertensive. Among the antepartum and intrapartum complications, the current study shows a maximum number of patients 25(50%) were affected with anaemia and 17(34%) teenage mothers developed no complication. The current study showed that the majority of the adolescent delivered by C/S 18(36%), spontaneous onset of labour 17(34%) and induction given 15(30%). The most common overall indication for caesarean section was foetal distress (about 14%), followed by eclampsia (8%). Study showed that that 2(4%) of teenage mothers suffered from PPH, 2(4%) had PPE, 3(6%) had wound infection and 4(8%) had partial breast feeding. The current study also showed that the APGAR score of the baby at the first minute 27(54%) were greater than 7 and 23(46%) were less than 7. The maximum number of babies 29(58%) were between 2-2.5 kg, 14(28%) had very low birth weights and only 7(14%) of baby birth weights greater than 2.5 kg. Study showed 14(28%) of the babies developed birth asphyxia, 8(16%) had prematurity, 2(4%) had jaundice.
Conclusion: We observed low birth weight is a key predictor for fetal complication and child mortality. It may be due to babies born to adolescent mothers are likely to be premature, and hence, the incidence of low birth weight is higher in them.
Keywords: Obstetric Risk, Neonatal Consequences, Adolescent Pregnancy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Gynae and Obs, Monno Medical College and Hospital Manikganj, Dhaka, , Bangladesh. Email: |
Rahman S, Choudhury FH, Jahan N, Hasan MM, The Obstetric Risk and Neonatal Consequences of Adolescent Pregnancy. Obs Gyne Review J Obstet Gynecol. 2024;10(1):40-48. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/172 |


 ©
©