Placenta Previa in Scarred and Nonscarred Uterus and Its Effect on Maternal Fetal Outcome
Wahid F1*, Kulsum U2, Islam N3, Akhtar N4, Parveen T5, Sayeeda S6, Kulsum SU7
DOI:https://doi.org/10.17511/joog.2024.i01.03
1* Fatima Wahid, Assistant Professor, Dept of Fetomaternal Medicine, Bsmmu, Dhaka, Bangladesh.
2 Umme Kulsum, Assistant Professor, Dept Of Fetomaternal Medicine, BSMMU, Dhaka, Bangladesh.
3 Nilufar Islam, Assistant Professor, Dept Of Fetomaternal Medicine, BSMMU, Dhaka, Bangladesh.
4 Nahreen Akhtar, Professor, Dept Of Fetomaternal Medicine, BSMMU, Dhaka, Bangladesh.
5 Tabassum Parveen, Professor and Chairman, Depart of Fetomaternal Medicine, BSMMU, Dhaka, Bangladesh.
6 Syeda Sayeeda, Professor, Dept Of Fetomaternal Medicine, BSMMU, Dhaka, Bangladesh.
7 Syeda Ummay Kulsum, Assistant Professor, Obstetrics Gynecology, BSMMU, Dhaka, Bangladesh.
Introduction: The Placenta, the life support system of the foetus, when implanted in the lower uterine segment affects fetomaternal outcome adversely. Placenta previa when diagnosed in 2nd or 3rd trimester is associated with a series of complications. Placenta previa is a major cause of vaginal bleeding in late 2nd and 3rd trimester.
Objective: To compare feto-maternal outcomes in cases of placenta previa occurring in scarred versus non-scarred uteri.
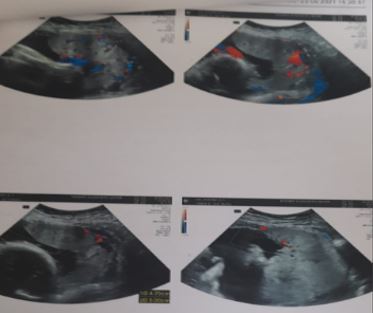
Methods: This study was a prospective observational study, conducted in the department of fetomaternal Medicine, BSMMU from January 2023 to June 2024. 60 cases analyzing placenta previa managed at a tertiary care centre. Patients were categorized into two groups: scarred uterus (n=46) and non-scarred uterus (n=14). Maternal outcomes including hemorrhage, hysterectomy rates, and perioperative complications were compared. Fetal outcomes such as gestational age at delivery, birth weight, and NICU admission rates were also evaluated.
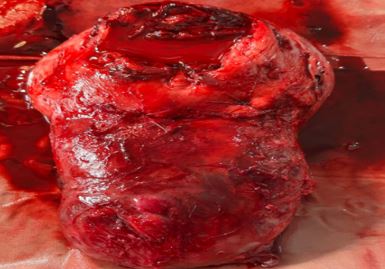
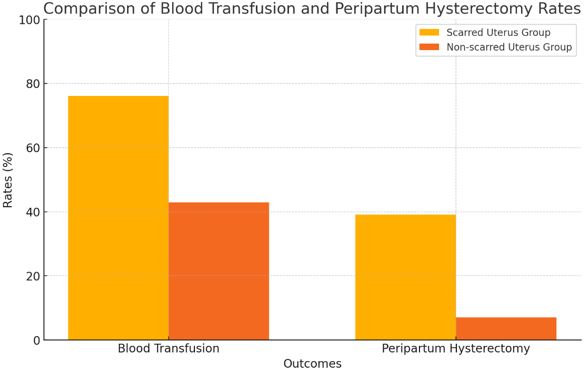
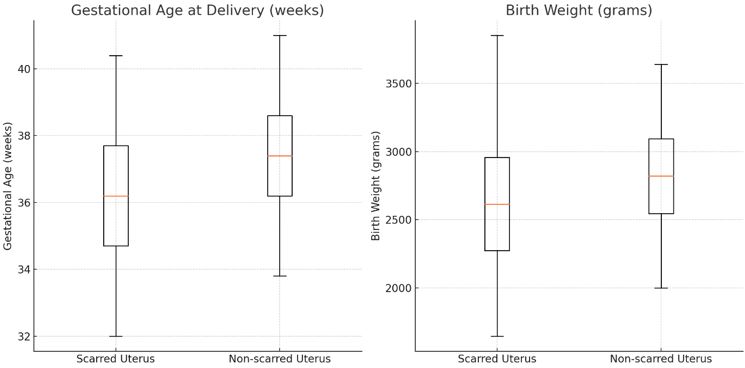
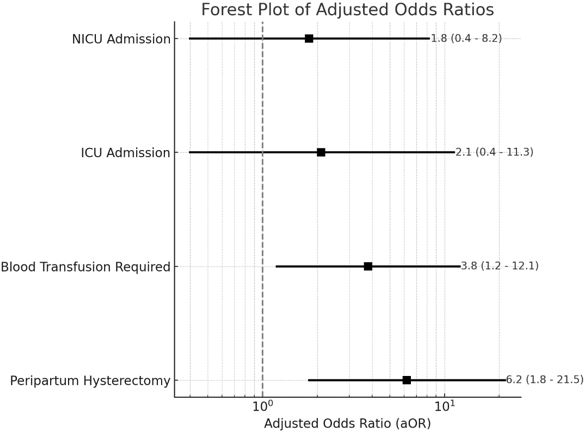
Results: Women with scarred uteri had significantly higher estimated blood loss (1850 ± 950 mL vs 1200 ± 650 mL, p=0.012), increased need for blood transfusion (76.1% vs 42.9%, p=0.021), and higher rates of peripartum hysterectomy (39.1% vs 7.1%, p=0.025) compared to those with non-scarred uteri. Placenta accreta spectrum disorders were more common in the scarred uterus group (37.0% vs 7.1%, p=0.038). After adjusting for confounding factors, having a scarred uterus remained an independent risk factor for peripartum hysterectomy (aOR 6.2, 95% CI 1.8-21.5, p=0.004) and for requiring blood transfusion (aOR 3.8, 95% CI 1.2-12.1, p=0.023). Fetal outcomes showed a trend towards being poorer in the scarred uterus group, but these differences did not reach statistical significance.
Conclusion: Placenta previa in the context of a scarred uterus is associated with significantly worse maternal outcomes, particularly in terms of hemorrhage, transfusion requirements, and hysterectomy rates.
Keywords: Placenta previa, cesarean section, uterine scar, maternal morbidity, placenta accreta spectrum, peripartum hysterectomy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Dept of Fetomaternal Medicine, Bsmmu, Dhaka, , Bangladesh. Email: |
Wahid F, Kulsum U, Islam N, Akhtar N, Parveen T, Sayeeda S, Kulsum SU, Placenta Previa in Scarred and Nonscarred Uterus and Its Effect on Maternal Fetal Outcome. Obs Gyne Review J Obstet Gynecol. 2024;10(1):16-24. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/169 |


 ©
©