The ambit of congenital malformations in the Kachchh district- a hospital-based study
Mehta D.1, Pawani C.2*, B Kukadiya S.3, Pandya N.4
DOI: https://doi.org/10.17511/joog.2020.i06.02
1 Dhwani Mehta, Third Year Resident, Department of Obstetrics and Gynecology, Gujarat Adani Institute of Medical Science, Kutch, Gujarat, India.
2* Charmi Pawani, Assistant Professor, Department of Obstetrics and Gynecology, Gujarat Adani Institute of Medical Science, Kutch, Gujarat, India.
3 Snehal B Kukadiya, Second Year Resident, Department of Obstetrics and Gynecology, Gujarat Adani Institute of Medical Science, Kutch, Gujarat, India.
4 Nimish Pandya, Profesoor and Head, Department of Obstetrics and Gynecology, Gujarat Adani Institute of Medical Science, Kutch, Gujarat, India.
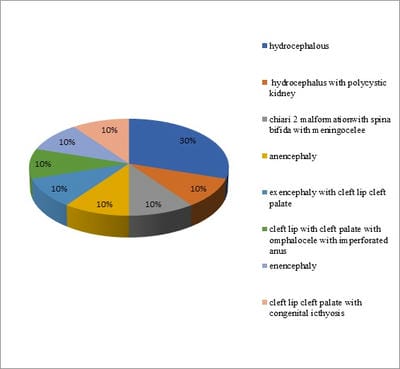
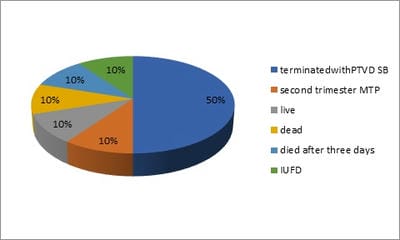
Background and Aim: Quantifying birth defects in a population is felt as a need as it helps inappropriate allocation of the health budget to tackle and reduce perinatal, neonatal, and infant mortality rates. Hence a study on congenital anomalies was undertaken in the region of Kachchh district. Material and Methods: Present cross-sectional study was performed on 10 patients diagnosed with having congenital malformed fetuses at tertiary care center- G.K. General Hospital, Bhuj, Kachchh district, Gujarat, India over three months – January, February, March 2019. Results: Mean age of the study participants were 22.3 years, most (70%) of the study participants were primigravida. Hydrocephalus was the most common birth defect among study participants. Eighty percentages (80%) of study participants had gross anomalies. Sixty percentages (60%) of participants had the outcome of termination. Conclusion: Congenital anomalies were in babies to mothers between 20-30 years of age. Once an anomaly is detected, various management options are to be discussed with the patients in consultation with a neonatologist, pediatric surgeon, and neurosurgeon when necessary.
Keywords: Birth defect, Congenital anomalies, Hydrocephalus, Pregnancy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Obstetrics and Gynecology, Gujarat Adani Institute of Medical Science, Kutch, Gujarat, India. Email: |
Mehta D, Pawani C, Kukadiya SB, Pandya N. The ambit of congenital malformations in the Kachchh district- a hospital-based study. Obs Gyne Review J Obstet Gynecol. 2020;6(6):114-119. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/122 |


 ©
©