Preoperative dexamethasone and intraperitoneal bupivacaine for postoperative pain relief
Gayam S.1*, Naduvinakeri K.2, Rajagopal M.3, Neelima C.4
DOI: https://doi.org/10.17511/joog.2020.i04.05
1* Susheela Gayam, Head of Department, Department of Obstetrics and Gynaecology, Vijay Marie Hospital and Educational Society, Hyderabad, Telangana, India.
2 Naduvinakeri K., Registrar, Department of Obstetrics and Gynaecology, Vijay Marie Hospital and Educational Society, Hyderabad, Telangana, India.
3 Meera Rajagopal, Senior Consultant, Department of Obstetrics and Gynaecology, Vijay Marie Hospital and Educational Society, Hyderabad, Telangana, India.
4 Neelima C., Senior Consultant, Department of Obstetrics and Gynaecology, Vijay Marie Hospital and Educational Society, Hyderabad, Telangana, India.
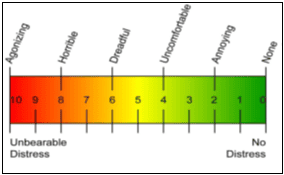
Introduction: Remarkable advancement in managing post-operative pain is made using various analgesics. Dexamethasone is a potent anti-inflammatory, analgesic, and anti-emetic agent and readily available, easy to administer, and a safe adjunct for postoperative analgesia. The intraperitoneal use of local anesthetics is known to improve postoperative pain. Objective: To assess the effectiveness of preoperative Dexamethasone combined with intra-peritoneal Bupivacaine for postoperative pain relief following surgery. Material and Methods: A prospective, randomized controlled study was done over a period of one year on 172 women scheduled for elective gynecological surgeries. The study group received Dexamethasone 8mg IV, 5 minutes prior to induction of anesthesia or before surgical incision, and intra-operatively 30ml of 0.25% Bupivacaine intraperitoneally under aseptic precautions. The control group received standard anesthesia as per the routine hospital protocol. Results: It was noted that the mean consumption of analgesic doses was significantly high in group B compared to group A (3.01±0.52 vs 1.46±0.83; p<0.001).The mean VRes scores in group A were significantly high compared to group B (2.95±1.01 vs 0.20±0.51; p<0.001). Conclusion: Dexamethasone combined with intra-peritoneal Bupivacaine is highly effective in reducing postoperative pain along with PONV.
Keywords: Preoperative Dexamethasone, Intraperitoneal Bupivacaine, Post-Operative pain relief
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Head of Department, Department of Obstetrics and Gynaecology, Vijay Marie Hospital and Educational Society, Hyderabad, Telangana, India. Email: |
Gayam S, Naduvinakeri K, Rajagopal M, Neelima C. Preoperative dexamethasone and intraperitoneal bupivacaine for postoperative pain relief. Obs Gyne Review J Obstet Gynecol. 2020;6(4):96-101. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/119 |


 ©
©