Sofa scoring tool for prediction of outcome in obstetric ICU at a tertiary care centre
Anand N.1*, Gokhale D.2
DOI: https://doi.org/10.17511/joog.2020.i02.01
1* Nupur Anand, Resident, Department of Obstetrics and Gynaecology, Medical College Baroda, Baroda, Gujarat, India.
2 A V. Gokhale, Head of Department, Department of Obstetrics and Gynaecology, Medical College Baroda, Baroda, Gujarat, India.
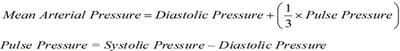
Introduction: Maternal deaths are defined by the WHO as the death of a woman while she is pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes. The Sequential Organ Failure Assessment (SOFA) score is one of the tools to evaluate the degree of organ failure in the patients leading to morbidity or mortality. Aims and Objectives: To validate that SOFA score can be used to know the prognosis of patients in obstetric ICU and to decide treatment accordingly. Materials and Methods: Organ failure was evaluated according to the maximum score for each one of its six components and the total SOFA score was calculated. The study was conducted in the Dept of Obstetrics and Gynaecology, Medical college and SSG Hospital, Baroda from 1st September 2017 to 31st August 2018. Result: The SOFA score trend in the patients who recovered showed a significant decrease with respect to time whereas the SOFA score trend in the patients who expired showed a significant increase. Interpretation of the area under the ROC curve showed that the performance of the total maximum SOFA score was excellent (AUC 0.972; 95% CI: 0.917 to 0.995). Conclusion: Total SOFA score proved to be an effective tool for evaluating the severity and estimating prognosis in obstetric ICU.
Keywords: Maternal mortality, Obstetric ICU, SOFA Score
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Resident, Department of Obstetrics and Gynaecology, Medical College Baroda, Baroda, Gujarat, India. Email: |
Anand N, Gokhale AV. Sofa scoring tool for prediction of outcome in obstetric ICU at a tertiary care centre. Obs Gyne Review J Obstet Gynecol. 2020;6(2):32-37. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/96 |


 ©
©