Factors affecting the success rate of vaginal birth after cesarean section
Prabha J. S.1, N. Prema2*
DOI: https://doi.org/10.17511/joog.2020.i02.03
1 Sathya Prabha J., Assistant Professor, Department of Obstetrics and Gynaecology, Karpagam Faculty of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
2* Prema N., Associate Professor, Department of Obstetrics and Gynaecology, Karpagam Faculty of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
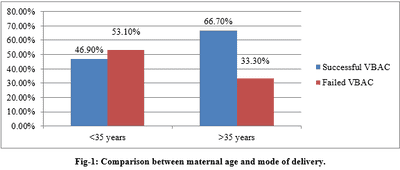
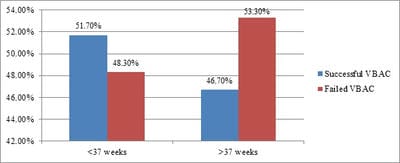
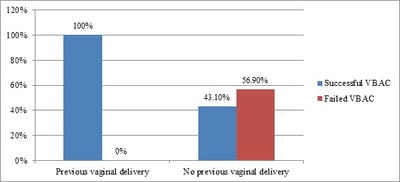
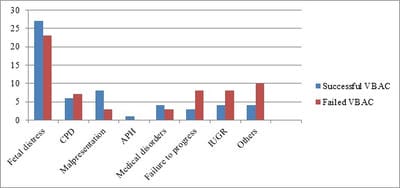
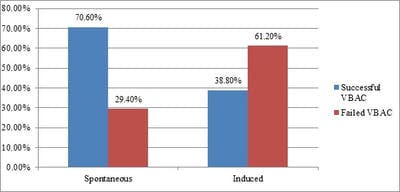
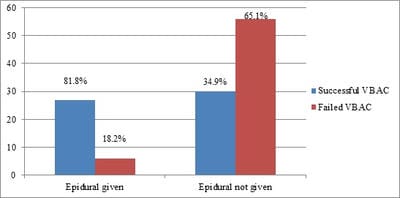
Introduction: The success rate of vaginal birth after cesarean section (VBAC) varies among institutions and health care providers. It is also affected by various antepartum, intrapartum factors as well as the difference in the obstetric population. Objectives: The main aim of the study is to determine the factors that affect the success rate of vaginal birth after cesarean section. This will help us to choose the right patients for VBAC thereby decreasing the complications of an emergency cesarean section. Methods: This is a prospective, cohort study done over a period of twelve months. Based on the patient's preference a total of 211 women were divided into two groups either a trial of labor after cesarean section (TOLAC) or elective repeat cesarean section (ERCS) group. VBAC group was compared with the failed trial of labor group to determine the factors affecting the success rate. Result: The success rate of VBAC was found to be 47.9%. About 15% of failed VBAC was due to the tendency to abandon a TOLAC midway. The success rate of VBAC increased in women with previous vaginal delivery and in those who went into spontaneous labor. Epidural was found to be safe to use in the trial of the labor group. Conclusion: Women with factors that increase the likelihood for vaginal delivery following cesarean section should be motivated well and referred to a tertiary center to improve the success rate as well as to reduce the maternal and fetal morbidity.
Keywords: Elective repeat cesarean section, Trial of labor after cesarean section, Vaginal birth after cesarean section
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Obstetrics and Gynaecology, Karpagam Faculty of Medical Sciences and Research, Coimbatore, Tamil Nadu, India. Email: |
Prabha JS, Prema N. Factors affecting the success rate of vaginal birth after cesarean section. Obs Gyne Review J Obstet Gynecol. 2020;6(2):46-52. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/92 |


 ©
©