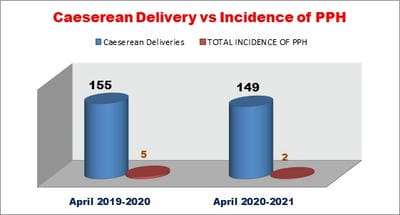
A Study to decrease the incidence of PPH in our hospital setting
Agrawal N.1*, Agrawal P.2
DOI: https://doi.org/10.17511/joog.2021.i04.01
1* Neelima Agrawal, Consultant, Department of Obstetrics and Gynaecology, Agrawal Hospital, Bhopal, Madhya Pradesh, India.
2 P. N. Agrawal, Consultant Respiratory and Critical care, Agrawal Hospital, Bhopal, Madhya Pradesh, India.
Objective: This study aimed to measure incidence, identify risk factors (pre‐existing or acquired) for PPH and to prevent progression to severe PPH. Methods: This is a prospective observational study. The causes are likely to be multifactorial with shifting demography and health status widely cited, e.g. age, obesity, comorbidity, multiple pregnancy and ethnicity. Results: Prepregnancy factors for PPH include age, ethnicity, BMI, previous PPH and assisted conception Conclusion: Prophylactic uterotonic agents in high-risk patients, use of intramuscular or intravenous oxytocin, timely application of B –lynch suture, adequate and timely arrangement of blood and blood factors can help prevent PPH.
Keywords: Postpartum haemorrhage (PPH), Maternal mortality, Uterotonic agents, B –lynch suture
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Consultant, Department of Obstetrics and Gynaecology, Agrawal Hospital, Bhopal, Madhya Pradesh, India. Email: |
Neelima Agrawal, P N Agrawal, A Study to decrease the incidence of PPH in our hospital setting. Obs Gyne Review J Obstet Gynecol. 2021;7(4):35-41. Available From https://obstetrics.medresearch.in/index.php/joog/article/view/141 |


 ©
©